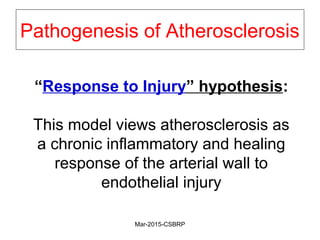
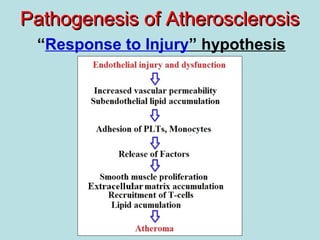
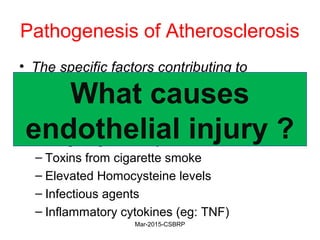
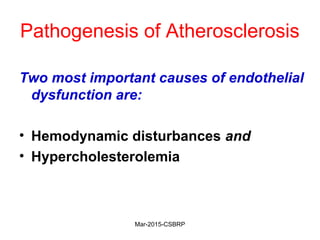
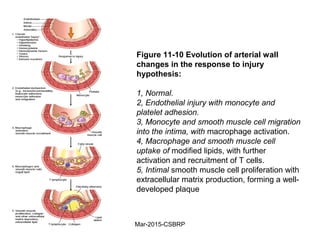
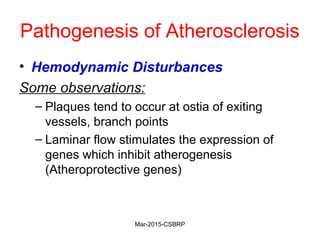
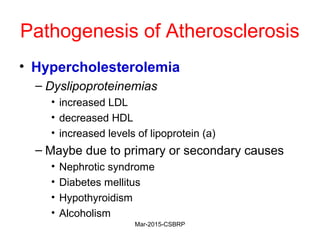
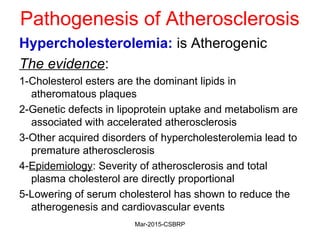
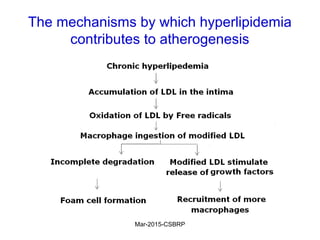
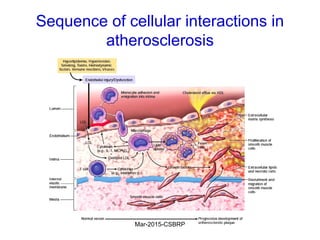
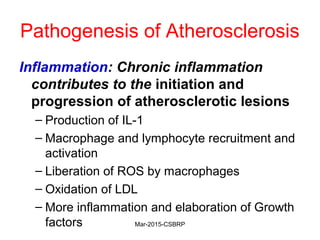
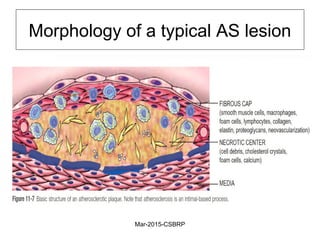
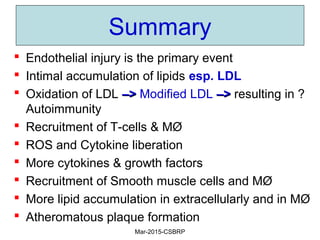
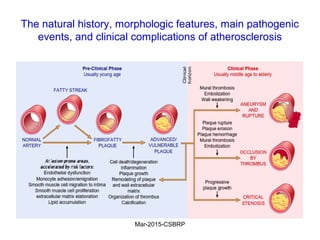
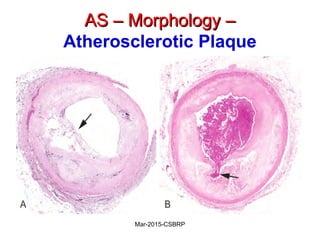
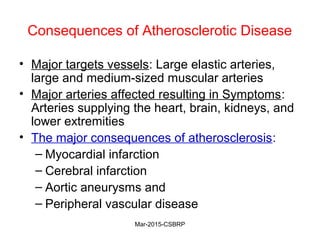
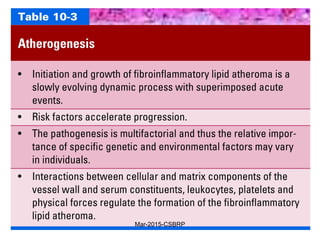
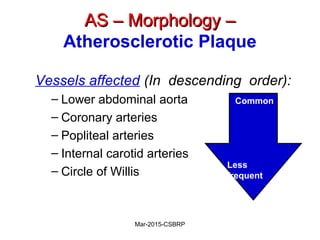
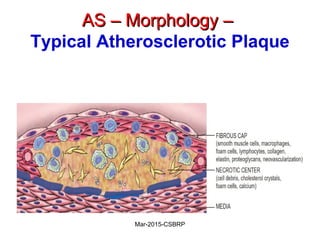
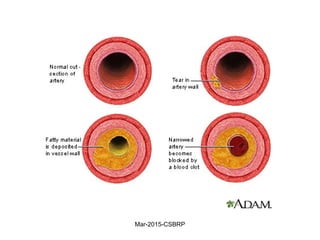
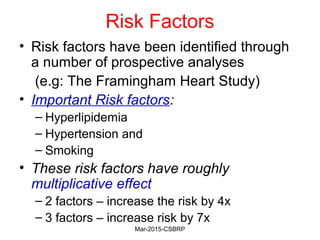
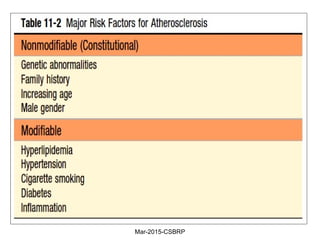
Atherosclerosis is a disease involving the hardening and narrowing of arteries from plaque buildup within the arterial wall. The document discusses the pathogenesis of atherosclerosis, which begins with endothelial injury from factors like smoking, inflammation, and hypercholesterolemia. This allows lipids like LDL to accumulate in the arterial intima, where they become oxidized and trigger an inflammatory response involving immune cells and cytokines. Over time, smooth muscle cells and macrophages are recruited, leading to the formation of atherosclerotic plaques containing lipids and cells that narrow the arteries. The document also covers risk factors, clinical implications like heart attacks, and theories of the disease process.


![Additional Risk Factors
• Inflammation
• Hyperhomocystinemia
• Metabolic syndrome
• Lipoprotein a [Lp(a)]
• Factors affecting hemostasis
• Other factors
Mar-2015-CSBRP](https://image.slidesharecdn.com/cvs-as-csbrp-151029114522-lva1-app6891/85/Cvs-as-csbrp-23-320.jpg)
![Additional Risk Factors
• Inflammation
• Hyperhomocystinemia
• Metabolic syndrome
• Lipoprotein a [Lp(a)]: Lp(a) levels are
associated with coronary and
cerebrovascular disease risk, independent
of total cholesterol or LDL levels
Mar-2015-CSBRP](https://image.slidesharecdn.com/cvs-as-csbrp-151029114522-lva1-app6891/85/Cvs-as-csbrp-28-320.jpg)
![Additional Risk Factors
• Inflammation
• Hyperhomocystinemia
• Metabolic syndrome
• Lipoprotein a [Lp(a)]
• Factors affecting hemostasis: Platelet-derived
factors, as well as thrombin—through both its
procoagulant and proinflammatory effects—are
increasingly recognized as major contributors to
vascular pathology
Mar-2015-CSBRP](https://image.slidesharecdn.com/cvs-as-csbrp-151029114522-lva1-app6891/85/Cvs-as-csbrp-30-320.jpg)
![Additional Risk Factors
• Inflammation
• Hyperhomocystinemia
• Metabolic syndrome
• Lipoprotein a [Lp(a)]
• Factors affecting hemostasis
• Other factors: lack of exercise;
competitive, stressful life style (“type A”
personality); and obesity
Mar-2015-CSBRP](https://image.slidesharecdn.com/cvs-as-csbrp-151029114522-lva1-app6891/85/Cvs-as-csbrp-31-320.jpg)