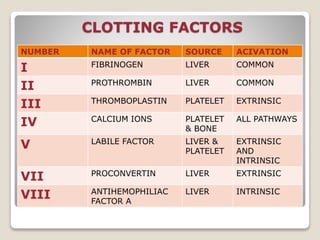
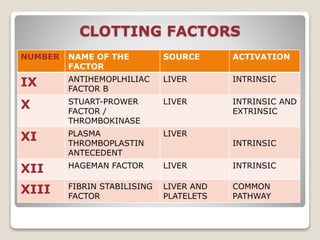
This document discusses bleeding, clotting, and related abnormalities. It covers the mechanisms of hemostasis, the clotting cascade, factors involved in clotting, causes of bleeding disorders, investigations for bleeding and clotting abnormalities, and treatment approaches. The key points are: bleeding can be external or internal; hemostasis involves vascular spasm, platelet plug formation, and blood clotting; clotting is a cascade of coagulation factors; abnormalities can cause excessive clotting (thrombosis) or bleeding; investigations include blood tests and imaging; treatment depends on the specific disorder but aims to replace any deficient clotting factors.