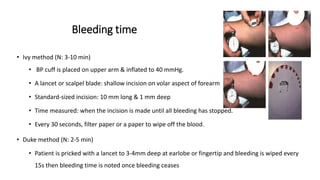
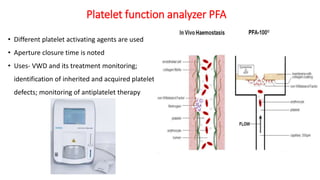
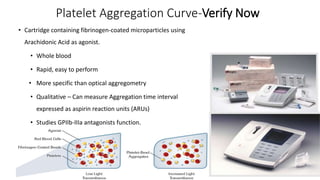
The document discusses the functions, disorders, and assessment of platelets, highlighting their role in hemostasis and various bleeding disorders, including congenital and acquired conditions. It details mechanisms of platelet activation, aggregation, and the significance of various assays for diagnosing platelet function disorders. Additionally, it addresses the complexities of different disorders affecting platelet count and functionality, with an emphasis on assessment methodologies such as light transmission aggregometry and flow cytometry.