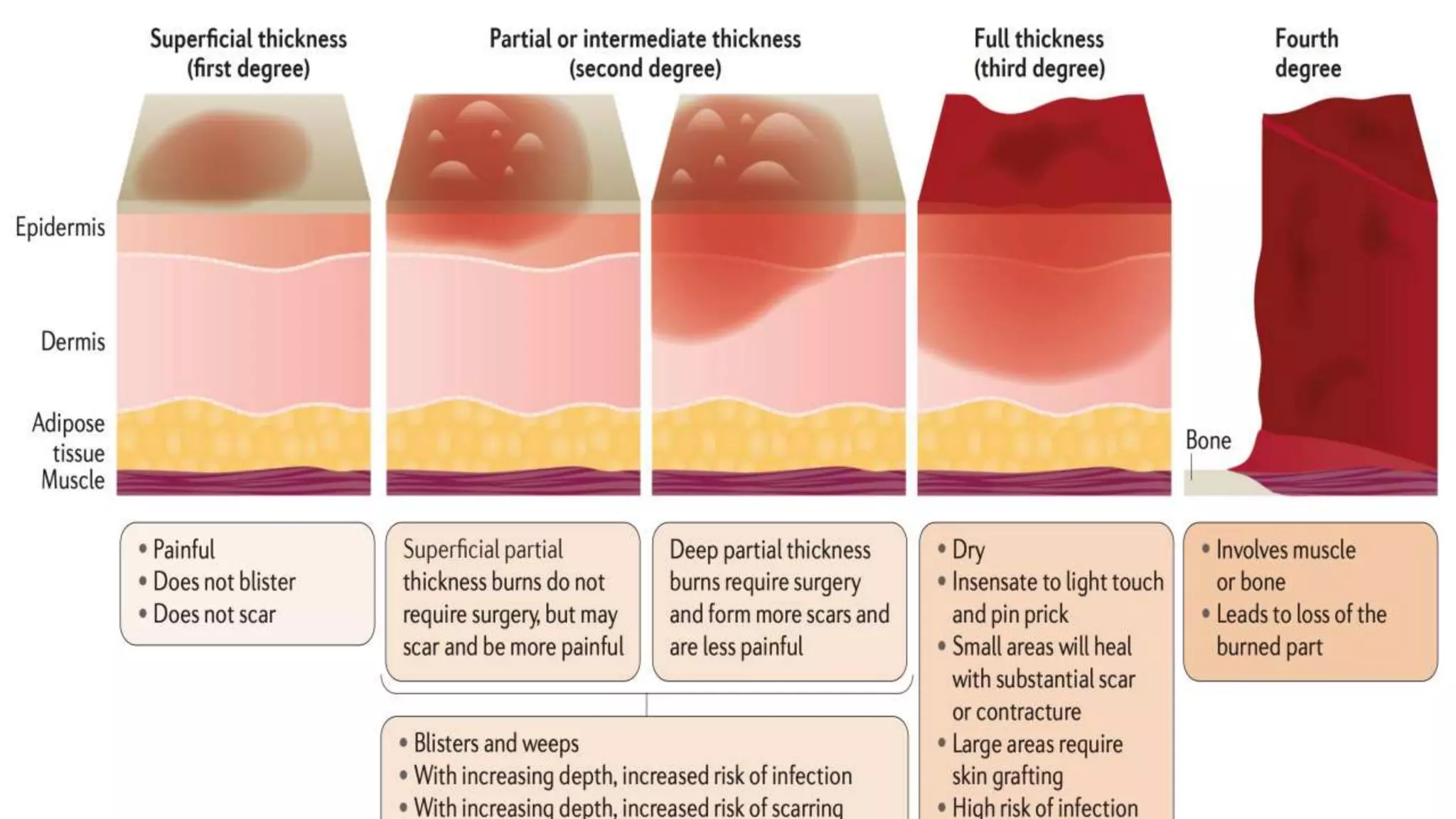
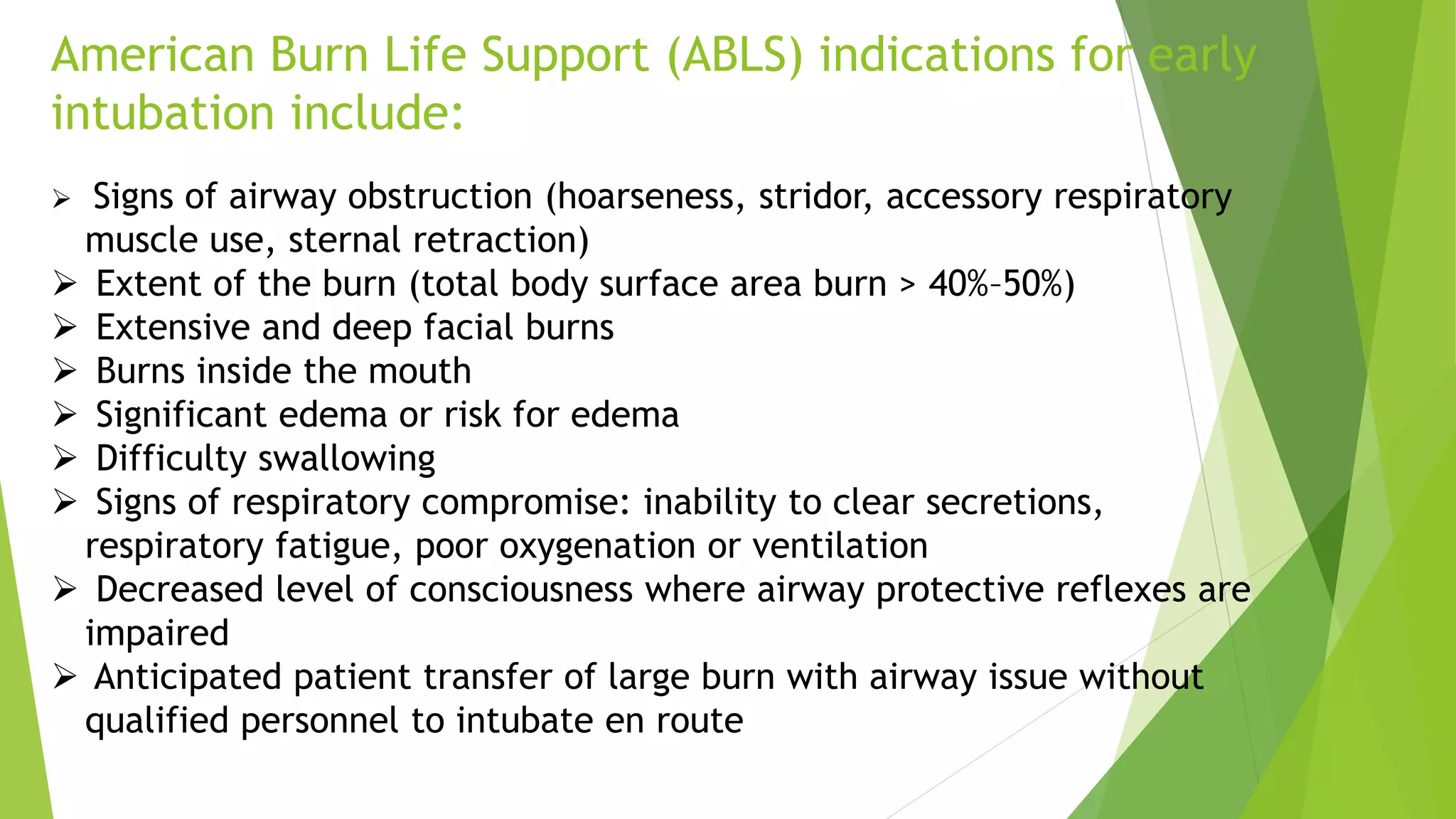
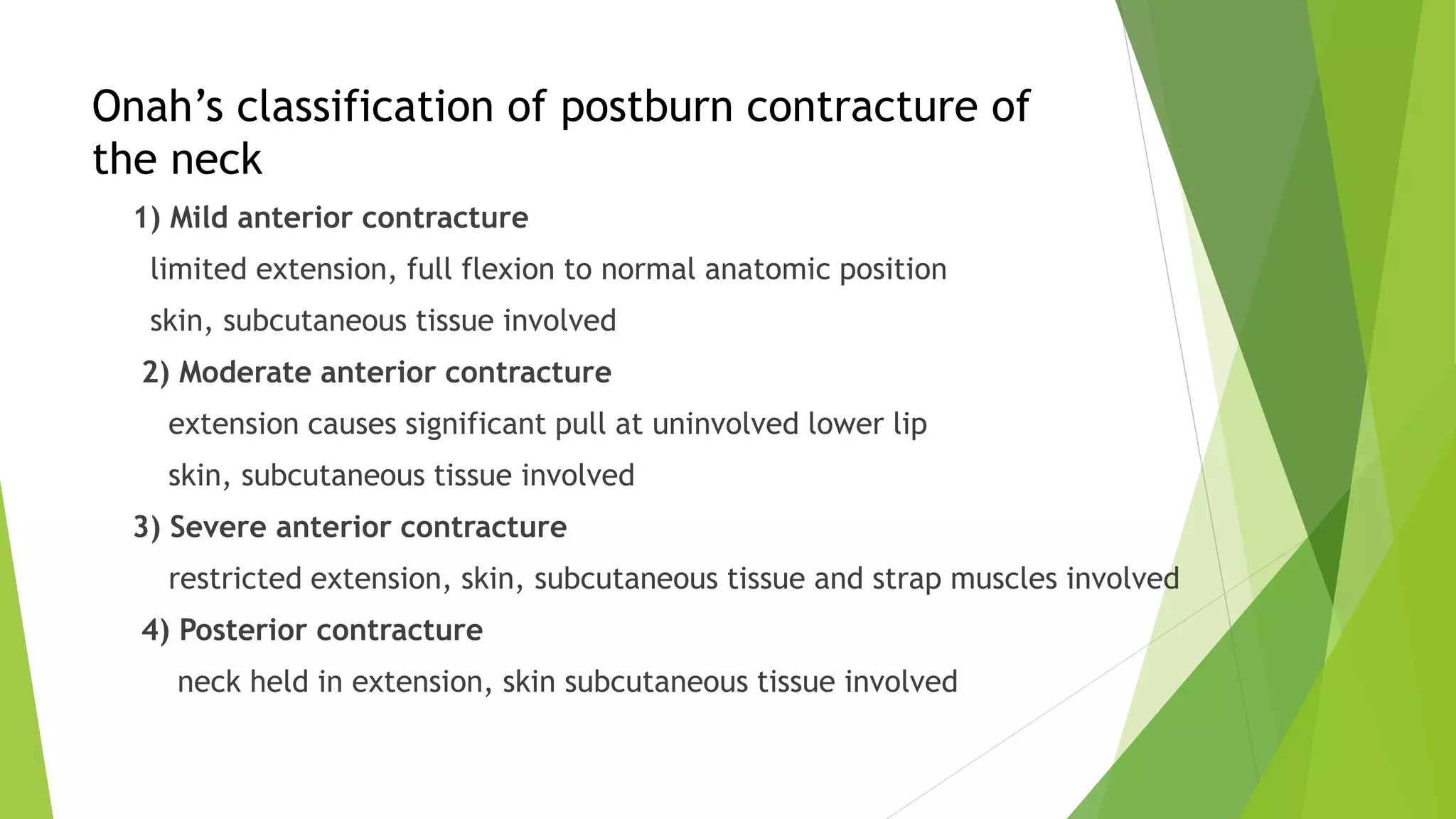
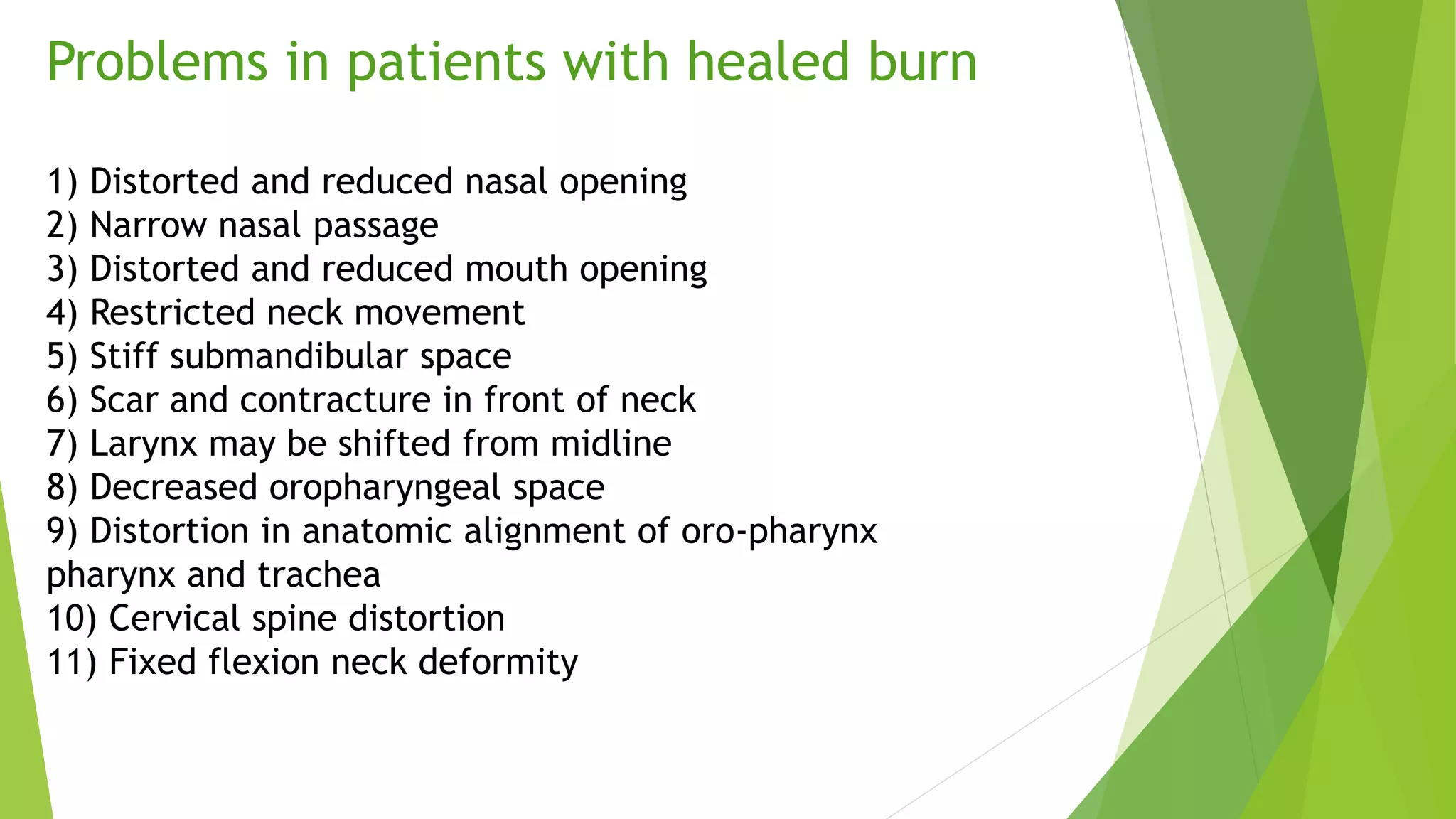
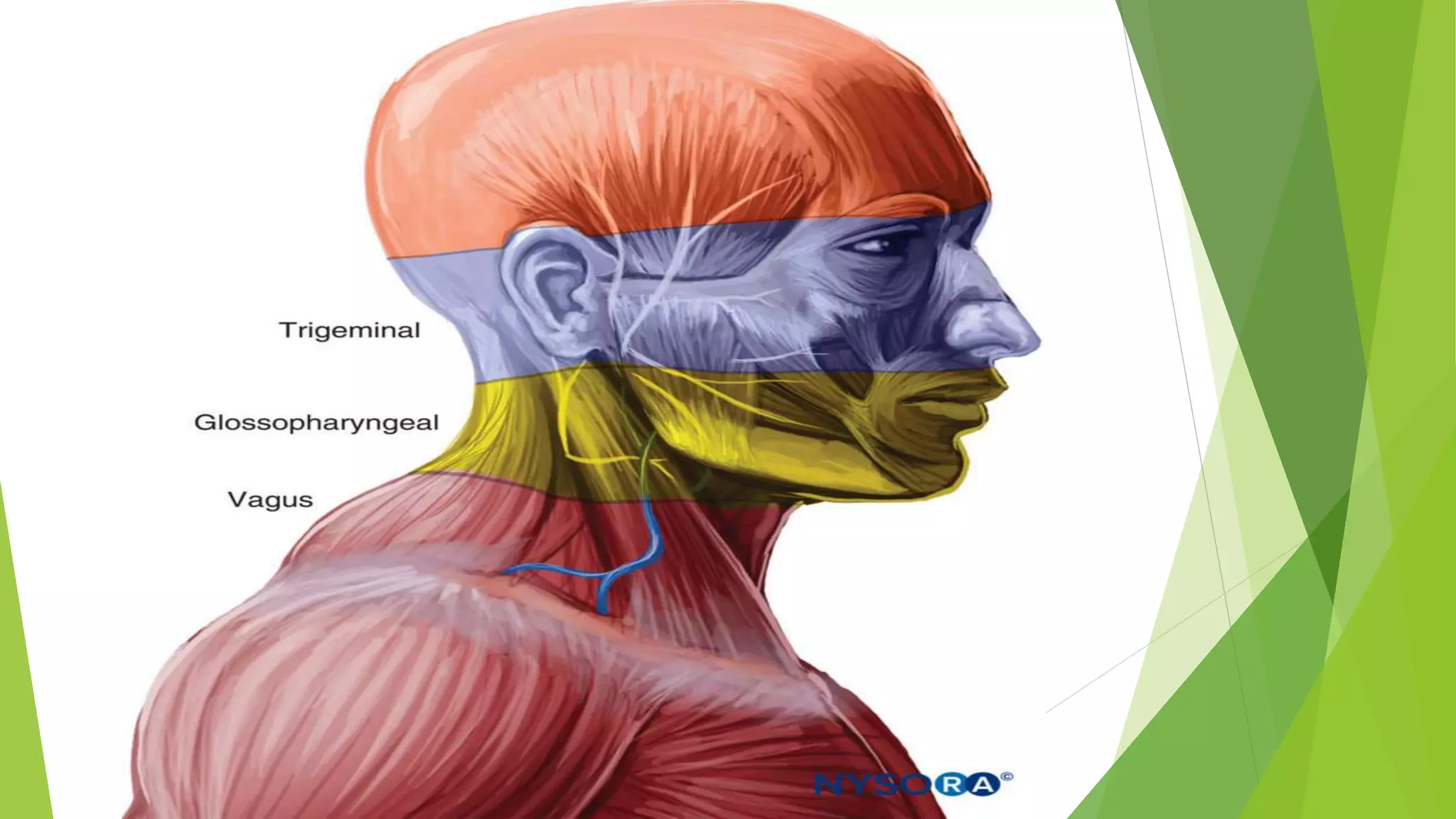
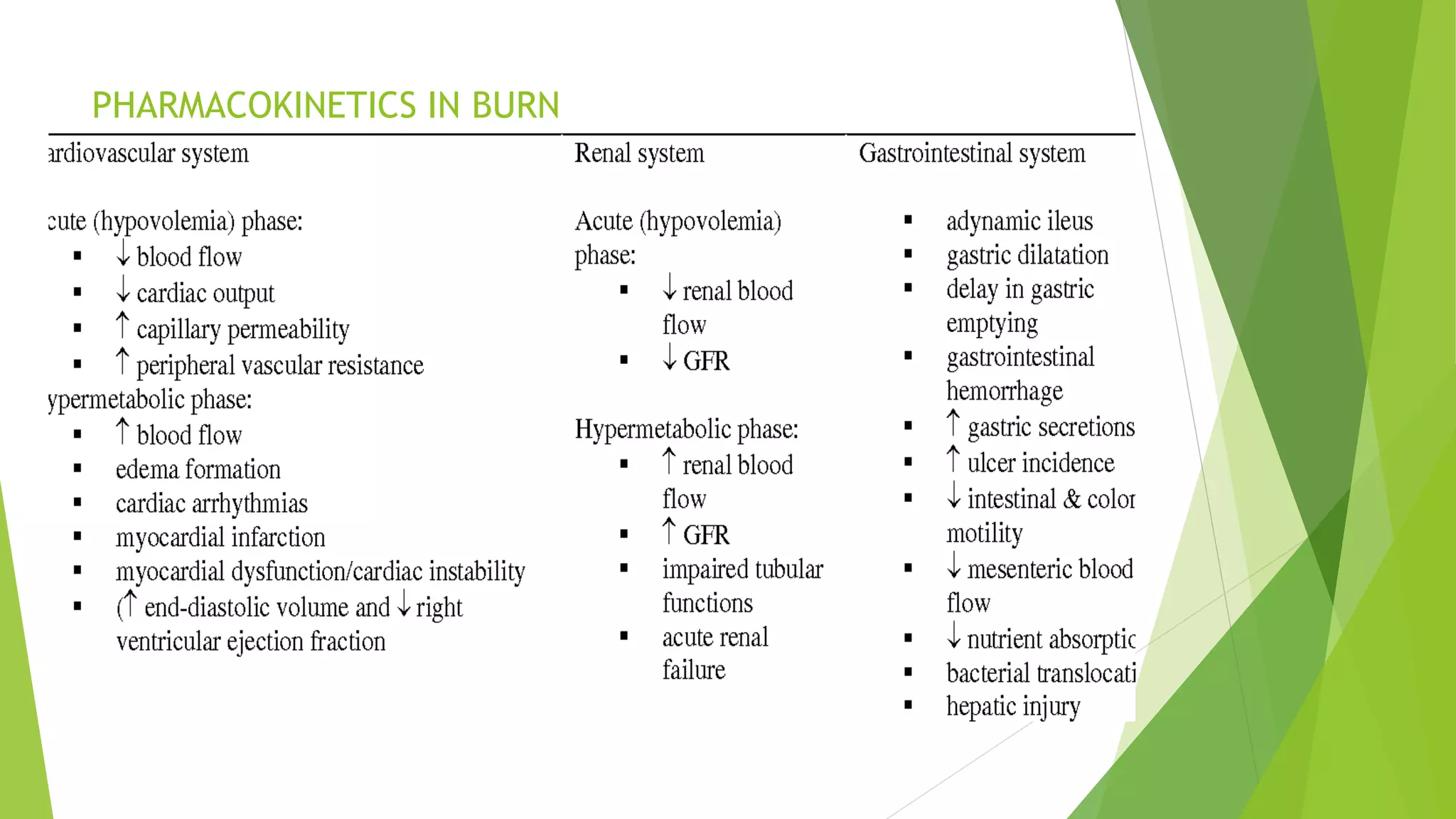
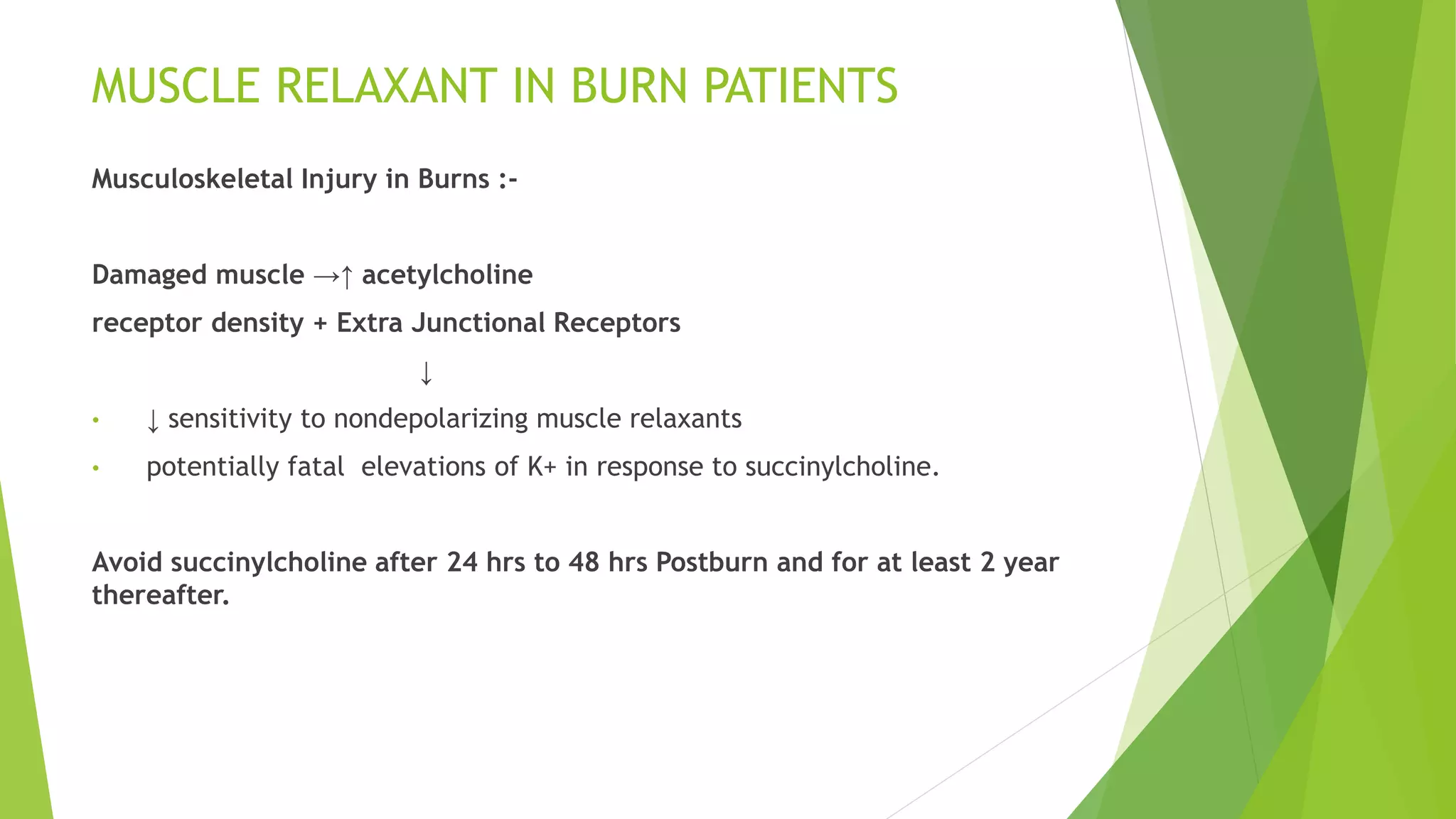
This document discusses considerations for airway management and anesthesia in burn patients. Major concerns include the extent and severity of burns, time since injury, and potential complications like infection and organ dysfunction. Early intubation is recommended for burns over 40-50% total body surface area or those involving the face, mouth or risking airway edema. Assessment of post-burn contractures that could distort airway anatomy is important. Awake fiberoptic intubation or other techniques may be needed. Muscle relaxants should be used cautiously in burns due to potential complications. Ketamine can provide hemodynamic stability and maintain airway reflexes in these high risk patients.