Normal Cardiac CT
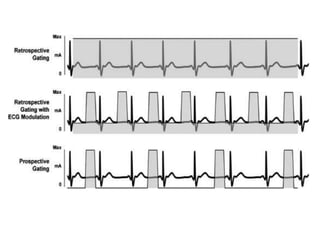
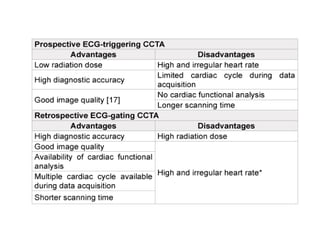
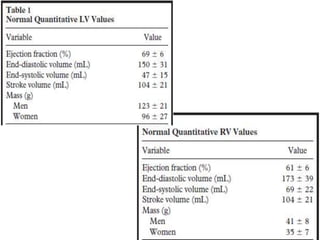
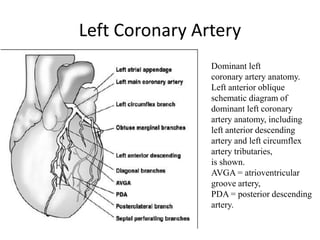
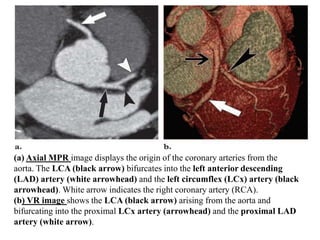
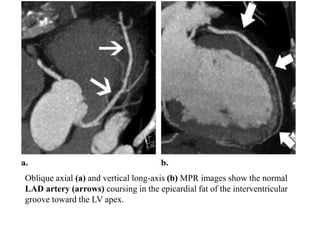
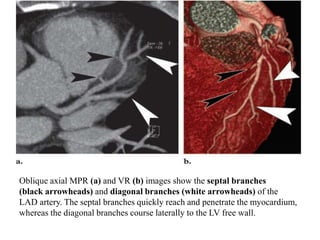
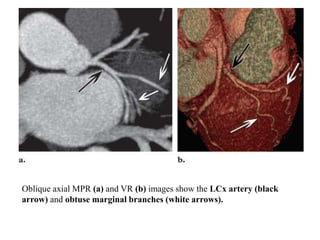
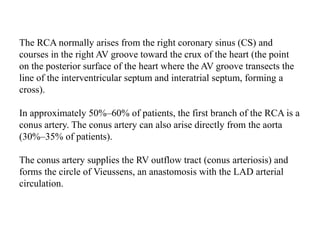
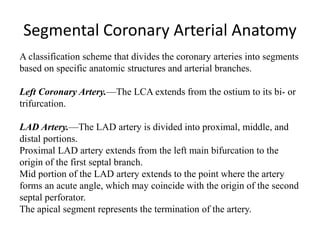
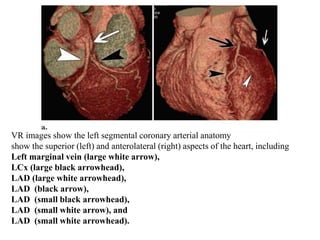
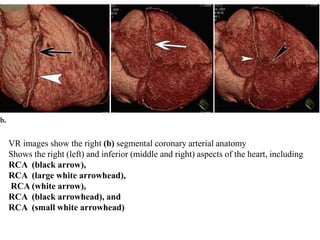
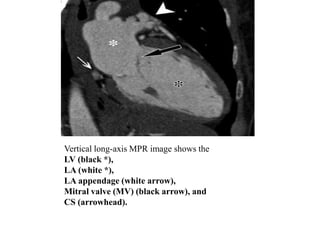
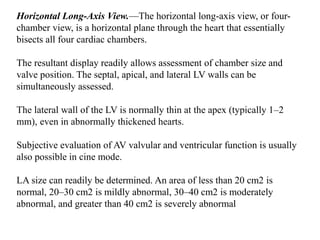
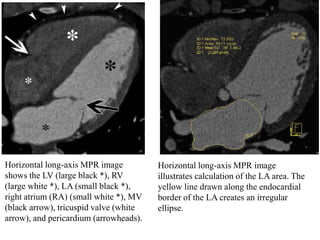
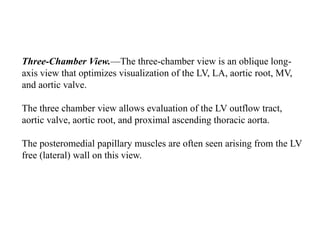
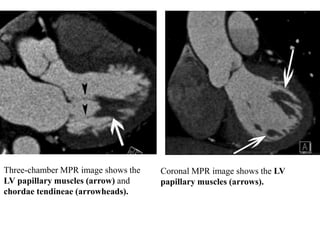
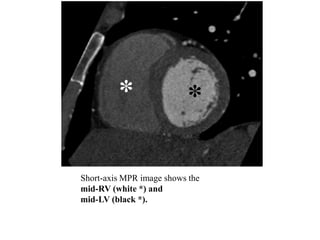
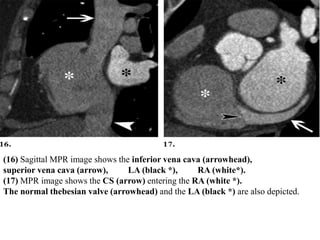
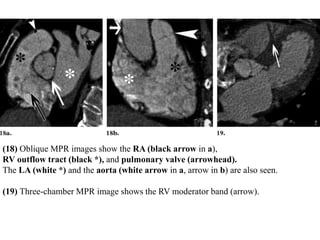
This document summarizes the key aspects of performing and interpreting a normal cardiac CT scan. It discusses the technique, including protocols for ECG gating and contrast injection. It then reviews the anatomy of the coronary arteries and important post-processing techniques like MPR, MIP, and VR. Segmental models for describing coronary artery anatomy are presented. Metrics for normal coronary artery diameter and left atrial area are provided. Common cardiac imaging planes and structures like the left ventricle and valves are also depicted.