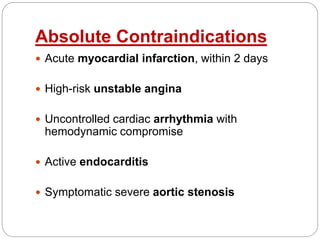
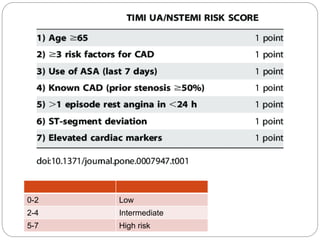
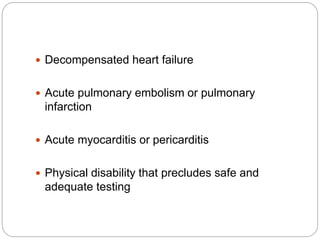
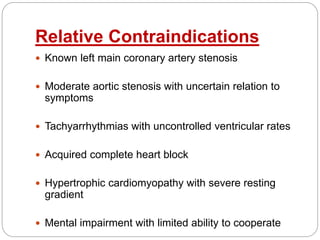
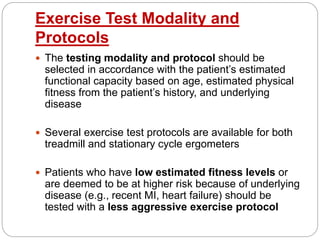
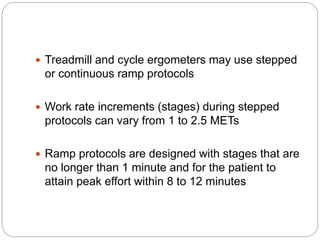
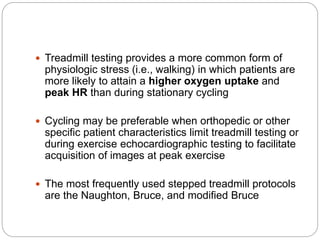
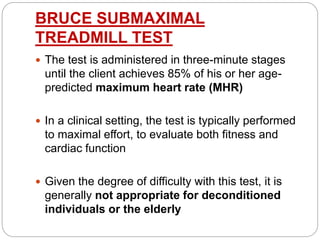
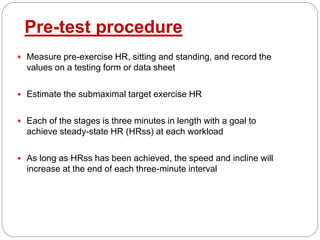
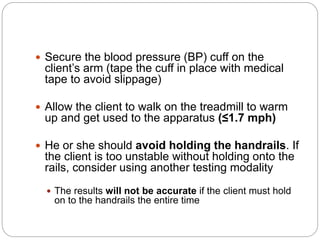
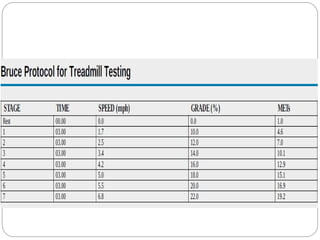
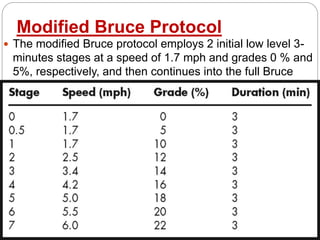
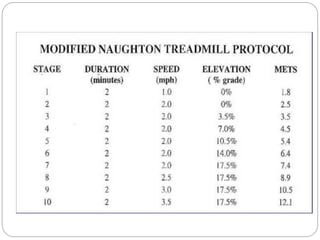
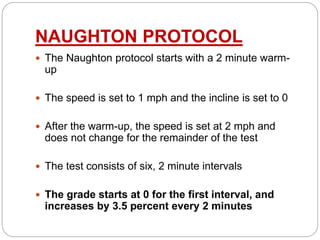
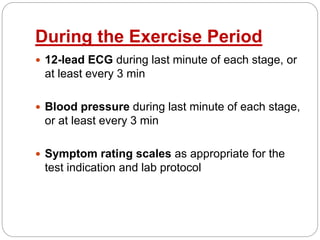
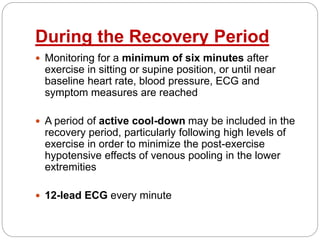
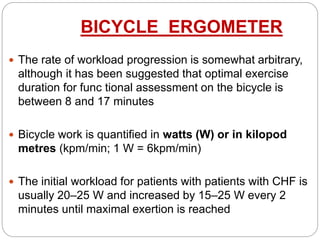
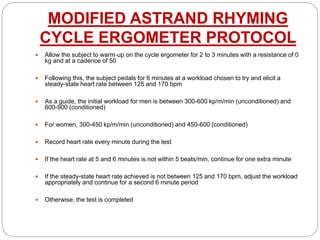
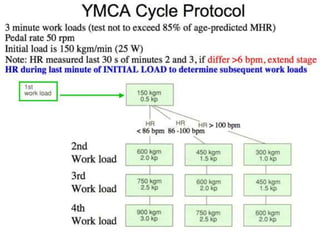
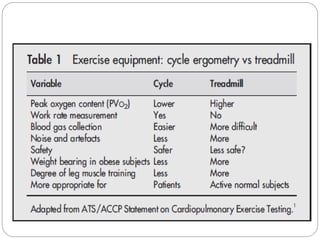
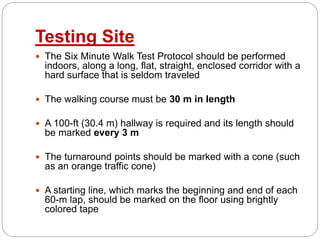
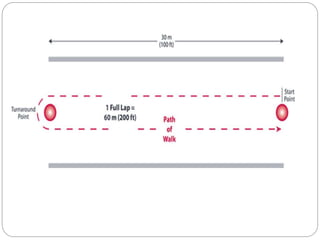
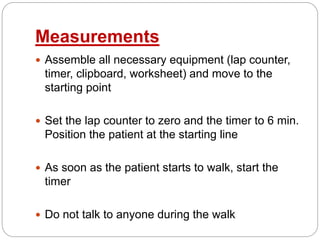
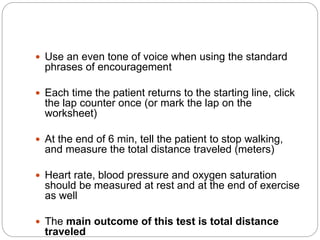
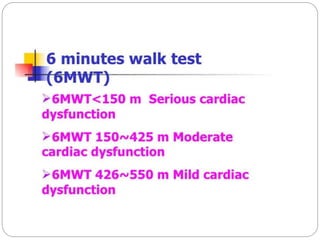
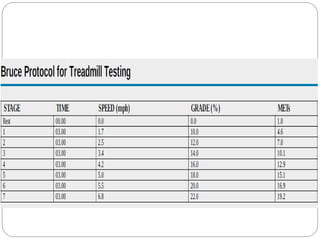
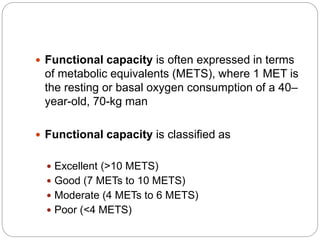
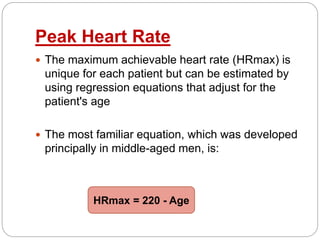
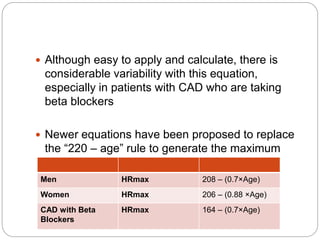
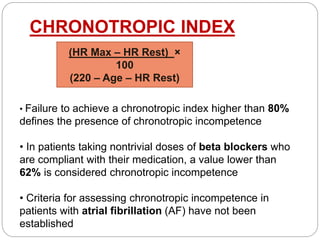
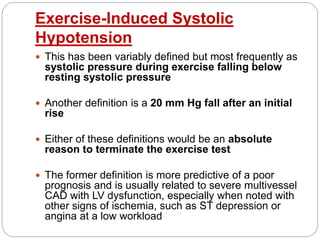
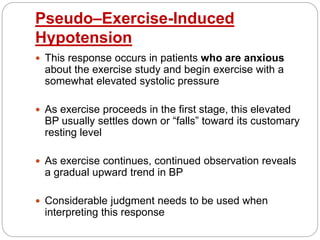
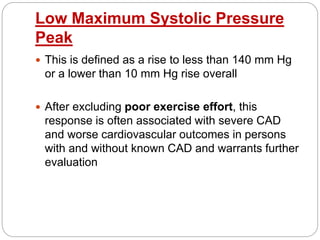
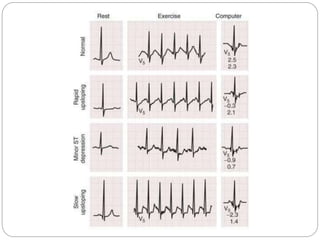
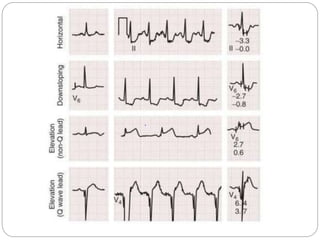
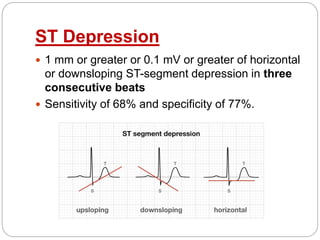
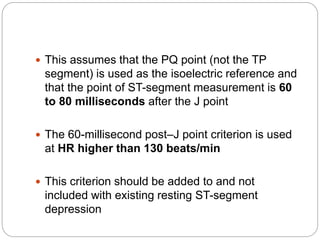
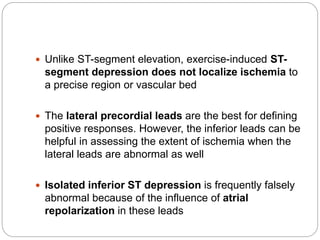
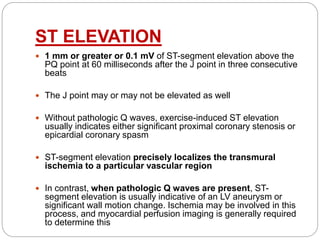
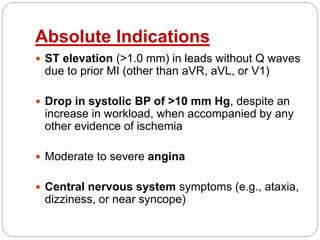
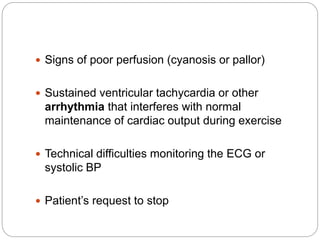
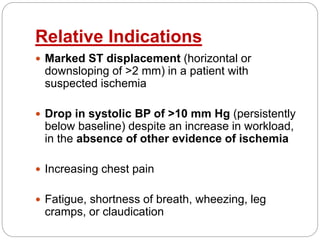
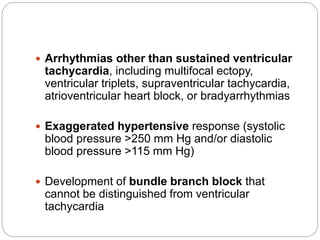
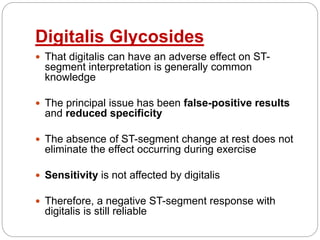
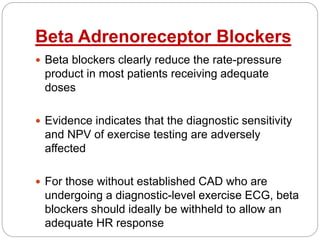
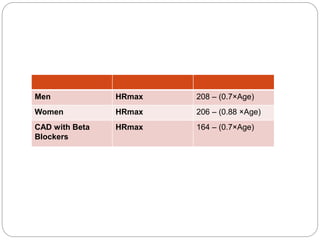
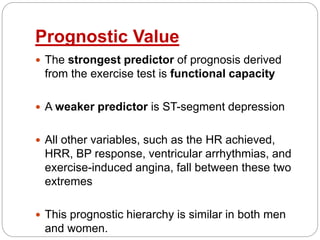
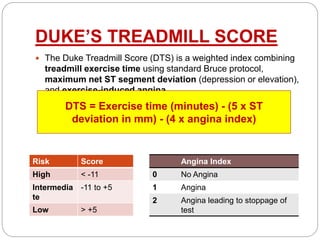
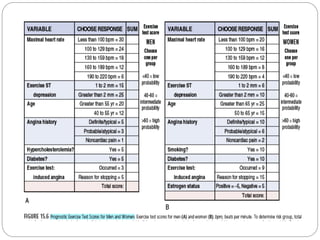
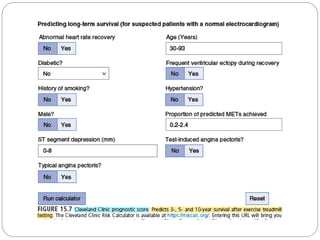
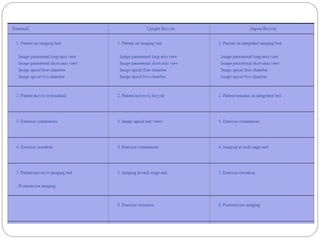
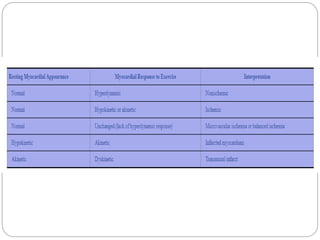
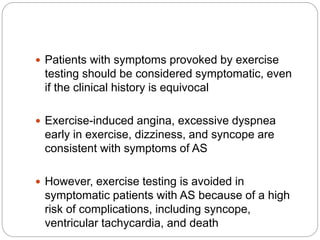
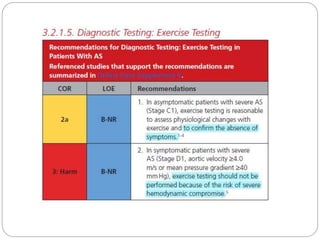
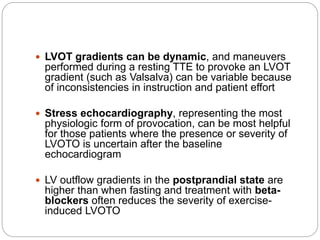
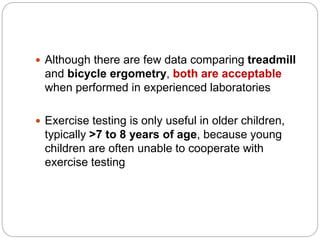
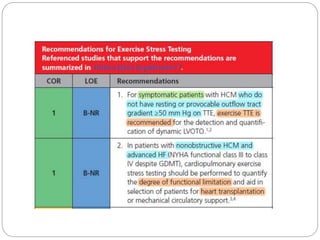
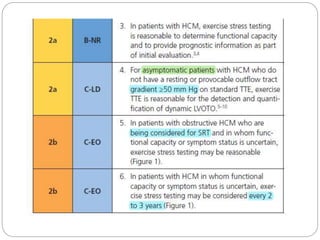
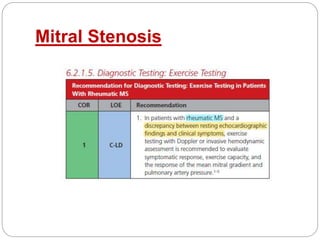
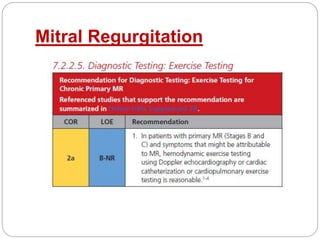
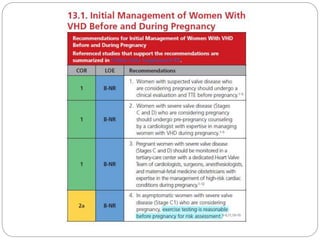
The document outlines absolute and relative contraindications for exercise testing in cardiology, highlighting conditions such as recent myocardial infarction and severe aortic stenosis. It details various exercise test protocols, including treadmill and cycle ergometer tests, emphasizing patient monitoring and assessment of functional capacity during testing. Additionally, it describes criteria for terminating tests based on ECG changes and blood pressure responses, along with considerations for interpreting results influenced by medications.