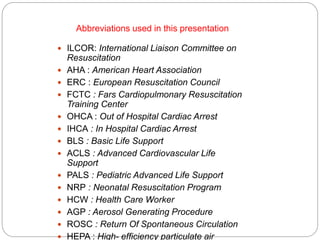
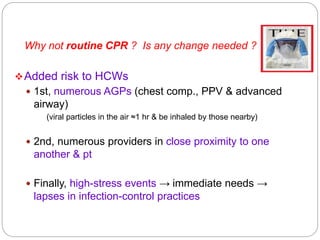
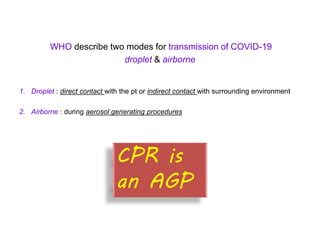
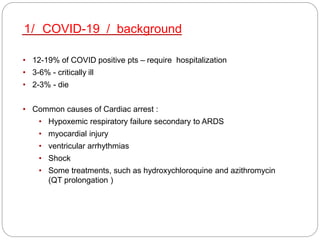
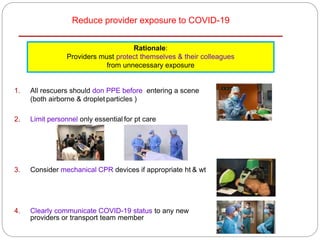
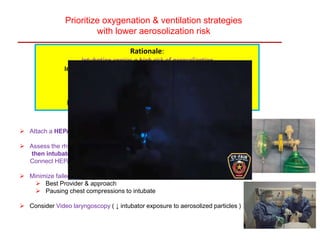
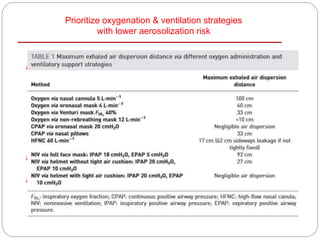
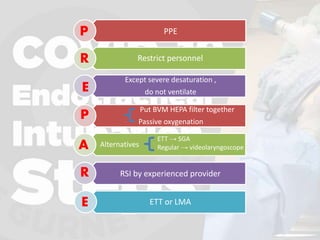
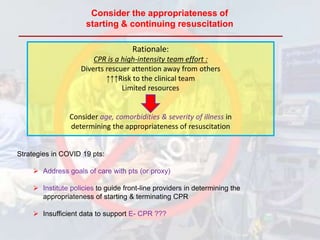
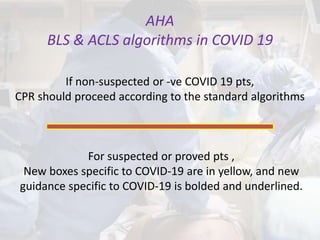
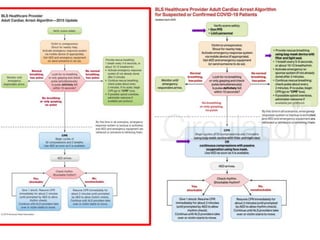
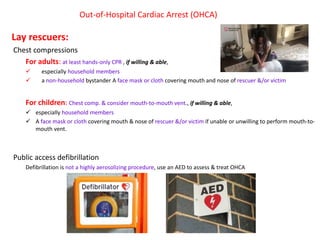
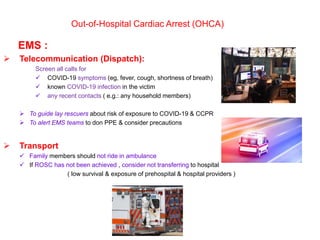
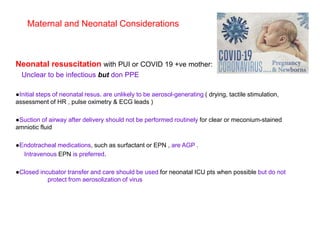
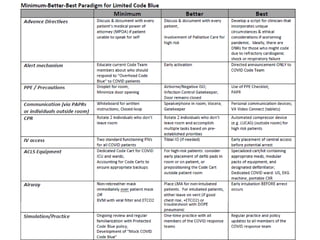
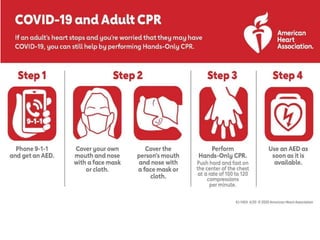
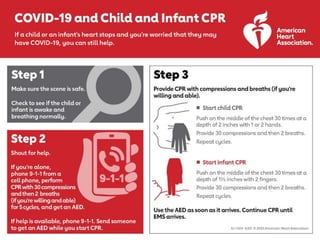
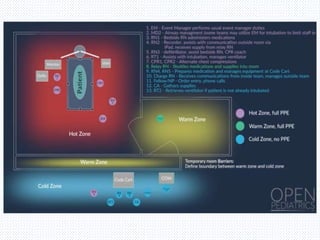
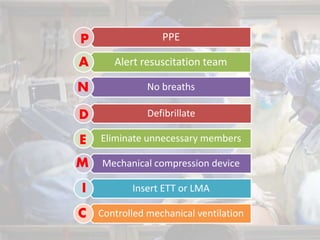
The document discusses CPR protocols during the COVID-19 pandemic, emphasizing the increased risks to healthcare workers due to aerosol-generating procedures. It outlines guidance from various resuscitation organizations on adapting CPR practices in both in-hospital and out-of-hospital settings, including the use of personal protective equipment (PPE) and considerations for patient assessment. Key recommendations include limiting personnel involved in resuscitation efforts, prioritizing communication about COVID-19 status, and modifying ventilation strategies to minimize aerosol exposure.