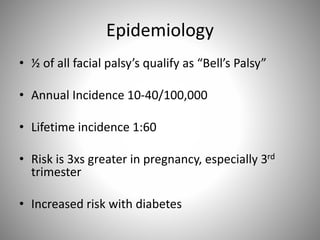
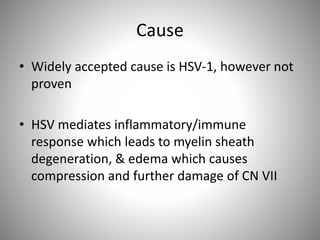
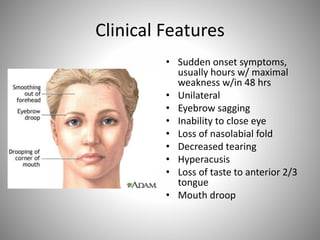
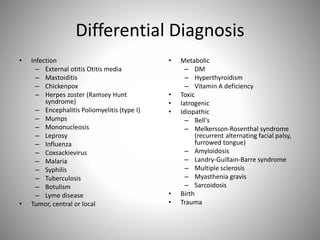
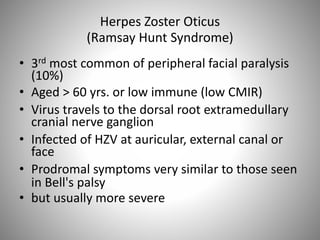
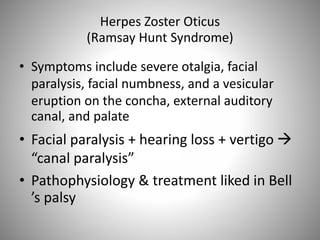
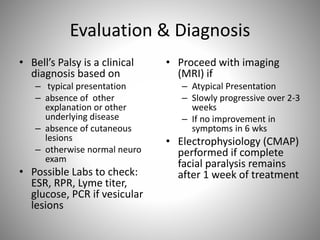
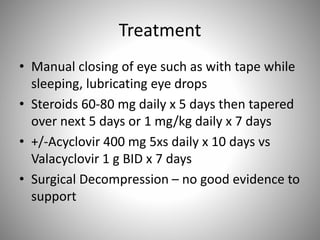
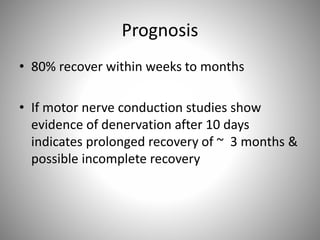
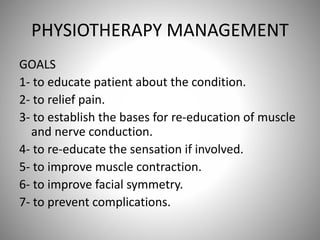
Facial palsy is paralysis of the 7th cranial nerve resulting in weakness of the muscles on one side of the face. It accounts for 75% of 7th nerve paralysis cases and is usually idiopathic (Bell's palsy). Imaging is not needed for typical cases but may be used to identify treatable lesions for atypical presentations. Treatment involves steroids, antivirals, eye protection, and physical therapy aimed at rehabilitating muscle function and symmetry over weeks to months with most cases fully recovering.