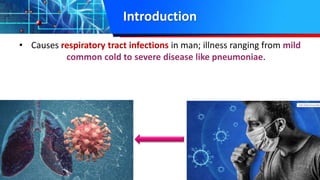
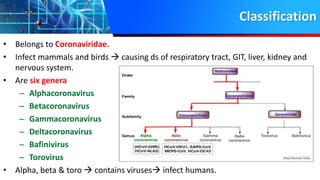
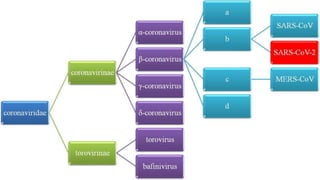
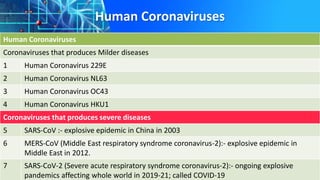
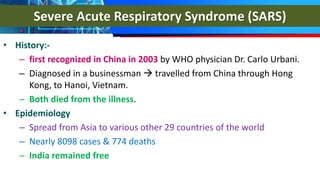
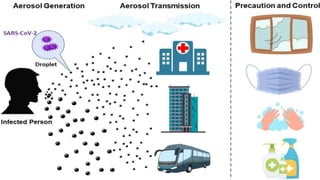
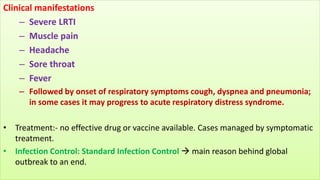
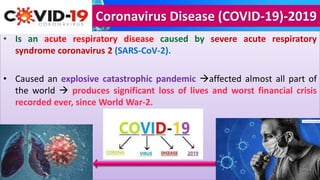
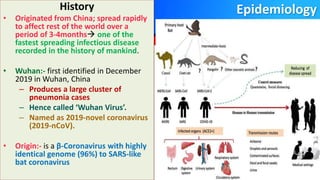
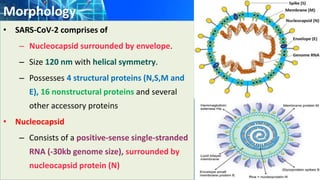
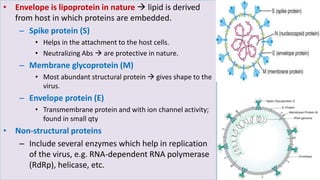
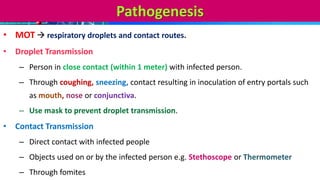
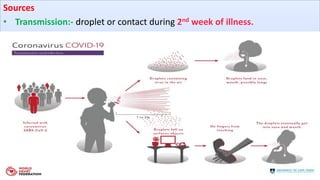
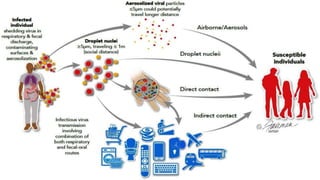
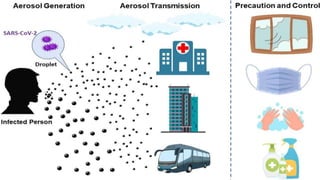
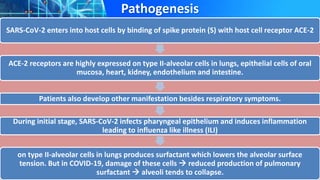
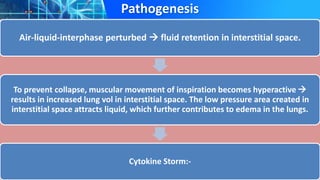
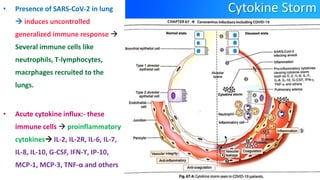
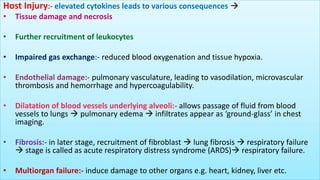
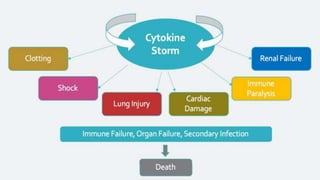
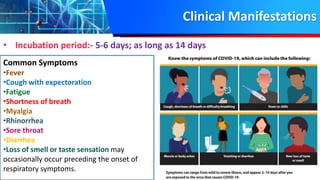
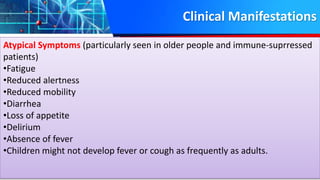
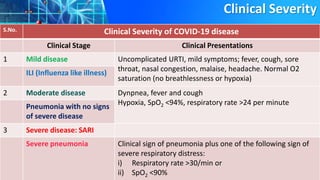
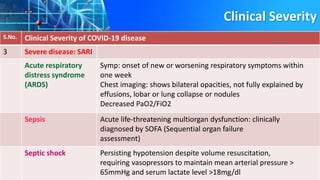
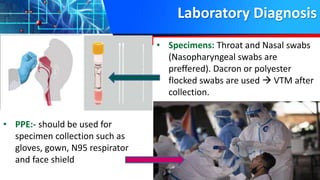
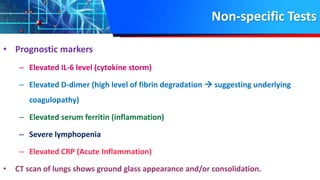
Coronaviruses can cause respiratory illnesses ranging from mild to severe like pneumonia. SARS-CoV-2, the virus that causes COVID-19, is an enveloped positive-sense RNA virus that binds to ACE2 receptors and primarily affects the respiratory system. It spreads via respiratory droplets and fomites. COVID-19 symptoms vary from mild to severe and can include fever, cough, fatigue, and shortness of breath. In severe cases it can cause acute respiratory distress syndrome due to a cytokine storm. Those at highest risk are elderly and those with pre-existing medical conditions.