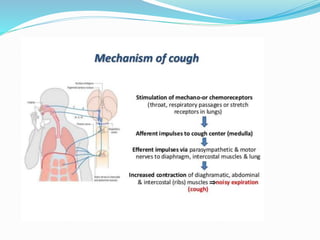
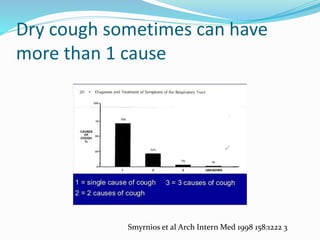
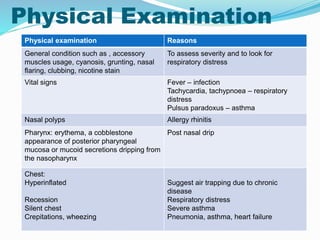
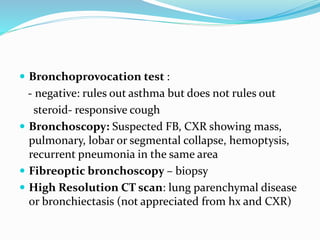
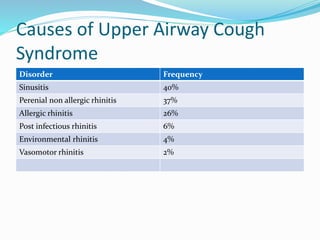
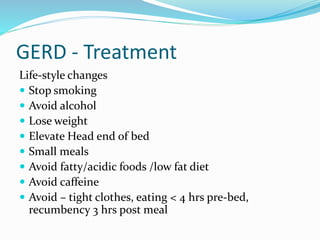
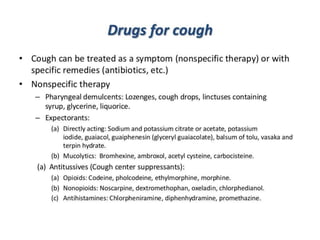
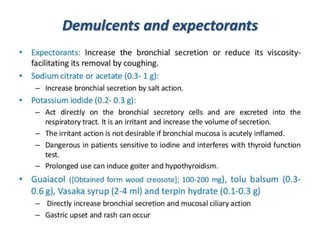
Dry cough is one of the most common symptoms prompting patients to seek medical care. A systematic diagnostic approach is recommended to determine the underlying cause. Common causes of acute dry cough include upper respiratory infections, while chronic dry cough may be due to asthma, COPD, GERD, or postnasal drip. A careful history and physical exam can provide clues to the etiology, and initial tests may include a chest x-ray, spirometry, and trial treatments targeting suspected conditions. Management involves treating the identified cause through lifestyle changes, medications, or other therapies.