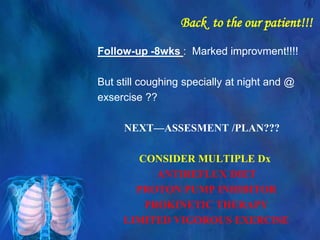
Based on the history and physical exam findings, this patient's chronic cough is most consistent with upper airway cough syndrome (UACS). Key factors include:
- Duration of cough >8 weeks
- Often dry cough, sometimes with white foamy sputum
- Worse with exercise, cold air, and at night
- Associated postnasal drip and throat clearing
- History of sinus problems
The physical exam is normal. Further workup and treatment based on the ACCP guidelines for UACS would be appropriate.