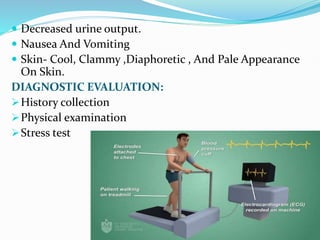
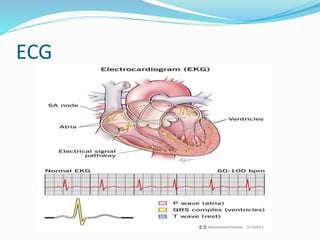
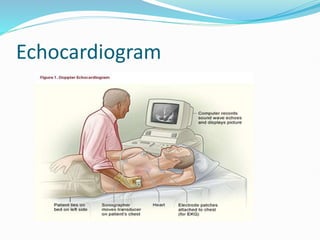
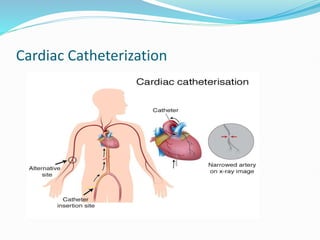
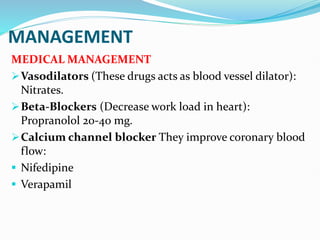
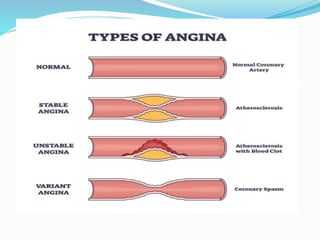
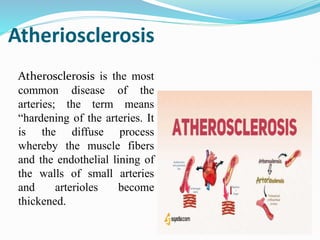
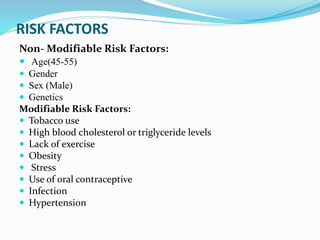
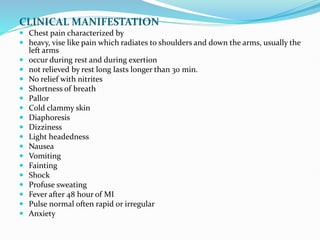
Coronary artery disease is caused by a narrowing of the coronary arteries due to atherosclerosis. It presents with chest pain and is associated with risk factors like smoking, high cholesterol, obesity, and lack of exercise. Diagnosis involves ECG, stress test, echocardiogram and angiogram. Treatment includes medications like nitrates, beta blockers, and statins as well as surgical procedures like angioplasty and bypass surgery. Nursing care focuses on monitoring vitals, managing pain and anxiety, and providing patient education.