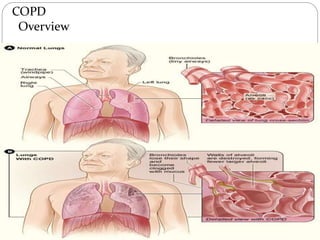
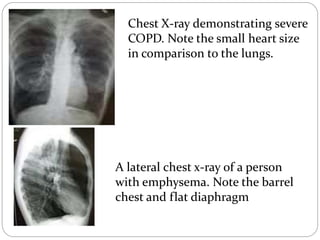
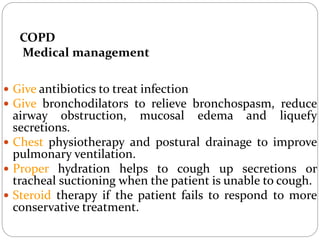
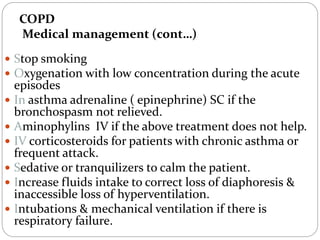
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by poor airflow. The main causes are smoking and air pollution. Symptoms include cough, sputum production, and shortness of breath. A diagnosis is made through pulmonary function tests showing obstructed airflow. Treatment focuses on smoking cessation, bronchodilators, oxygen therapy, and managing exacerbations.