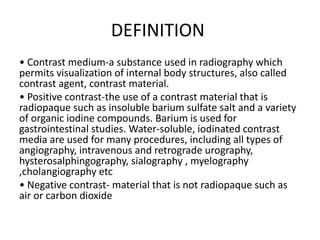
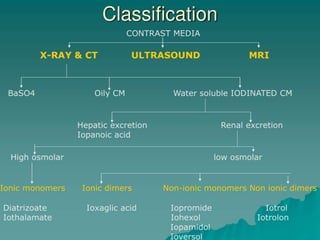
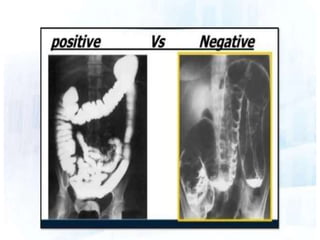
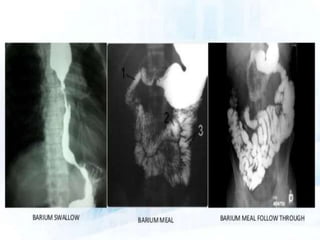
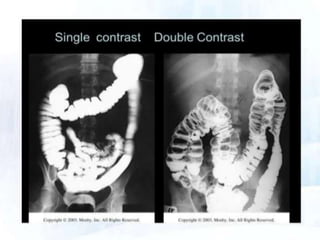
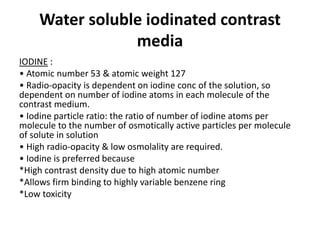
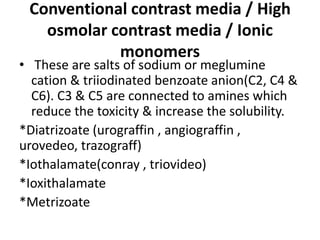
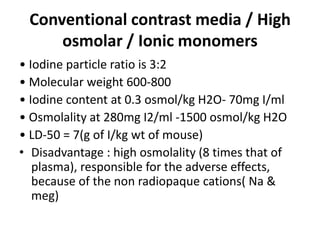
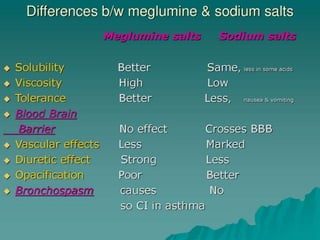
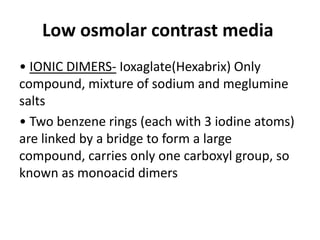
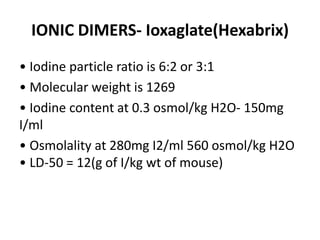
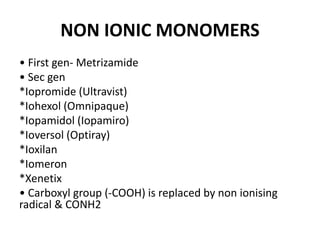
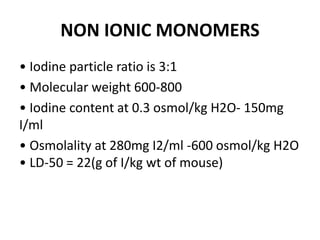
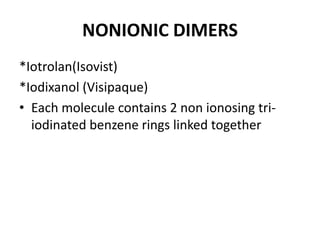
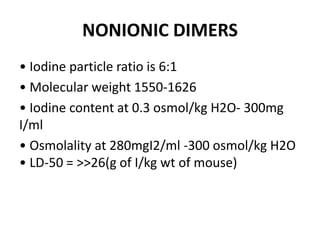
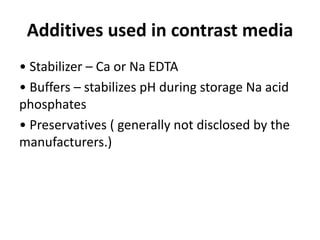
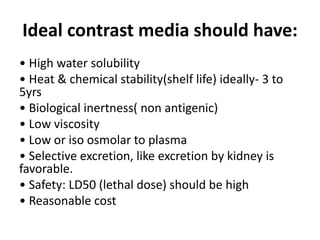
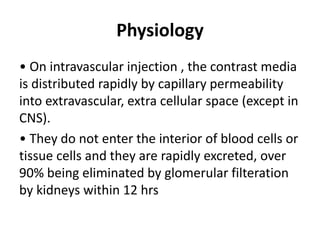
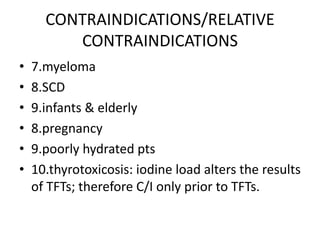
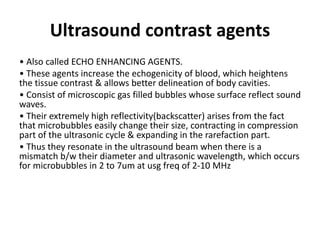
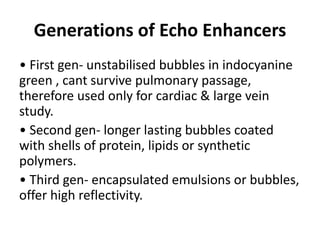
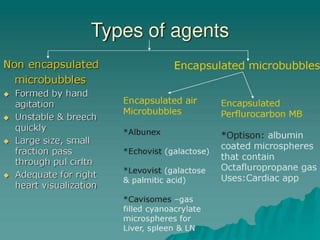
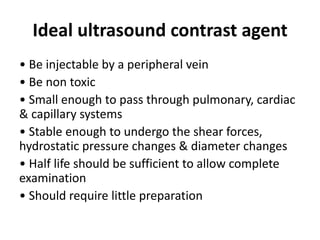
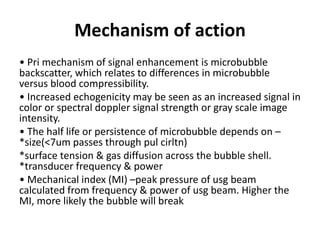
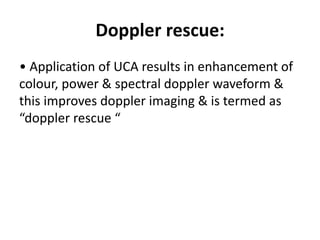
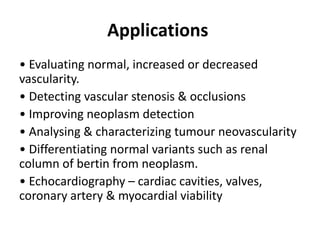
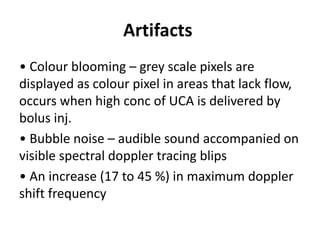
This document discusses various contrast agents used in medical imaging. It begins by defining contrast agents and describing their classification. It then focuses on water soluble iodinated contrast agents, describing their physiology and classifications including conventional high osmolar agents, low osmolar agents, and iso-osmolar agents. The document also discusses ultrasound contrast agents, their generations and mechanisms of action. It concludes by covering MR contrast agents such as gadolinium chelates and their uses and properties.