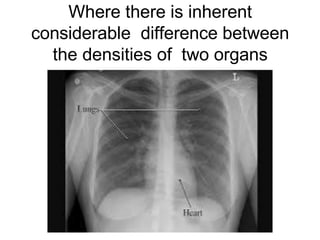
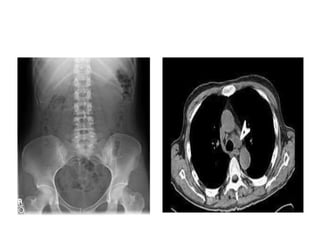
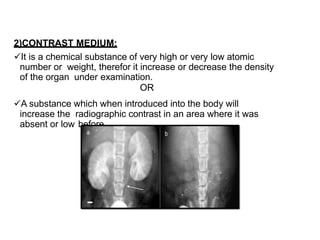
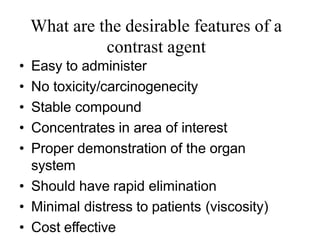
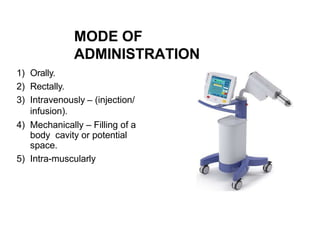
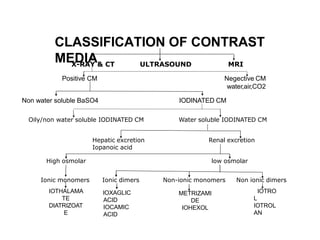
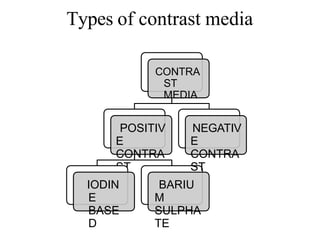
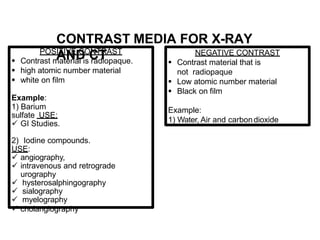
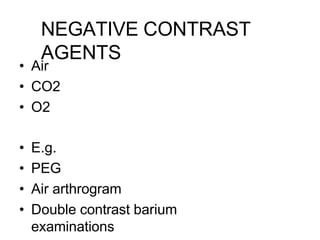
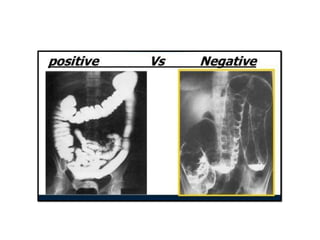
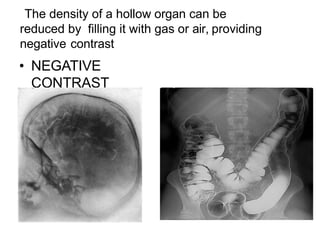
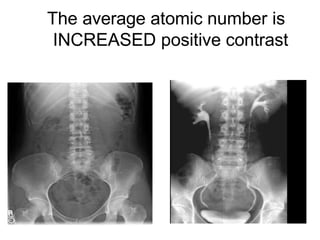
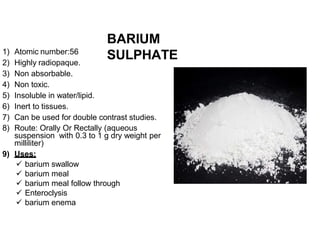
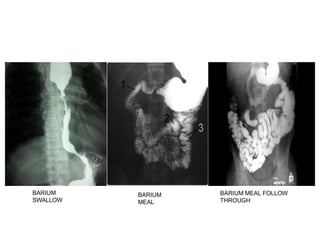
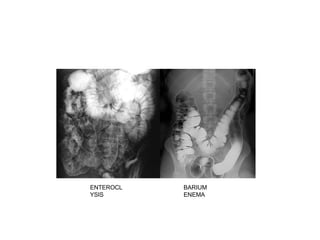
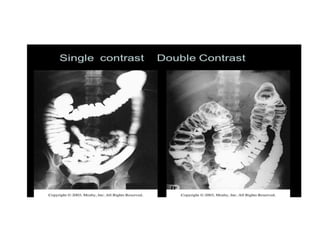
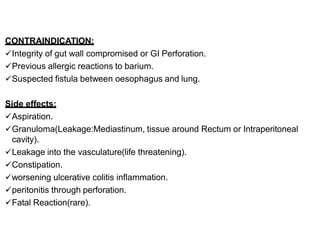
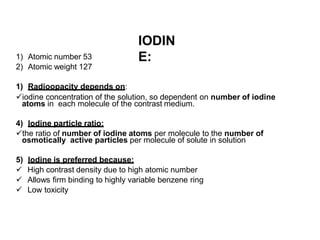
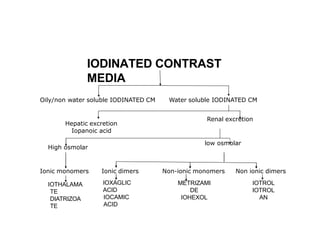
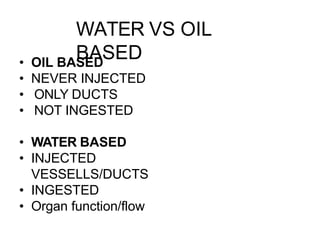
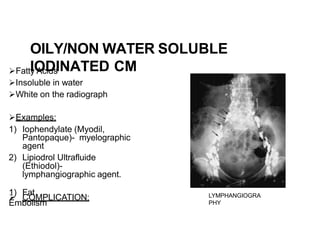
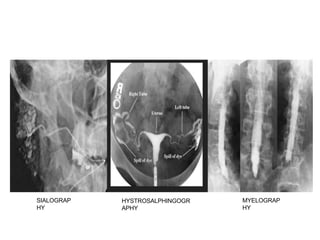
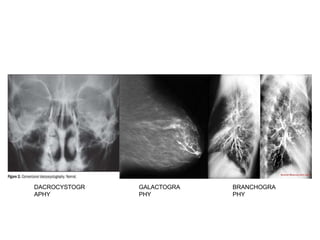
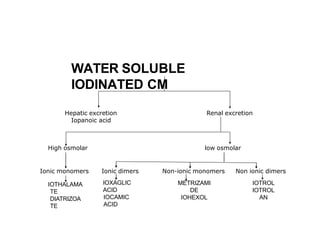
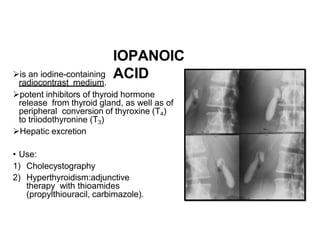
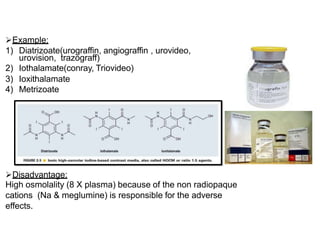
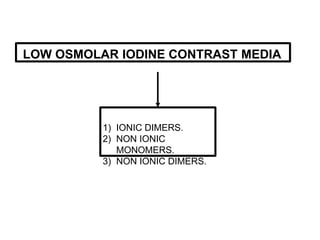
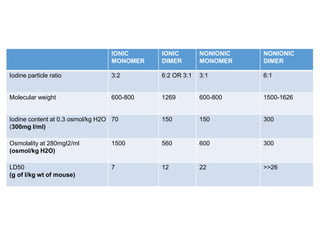
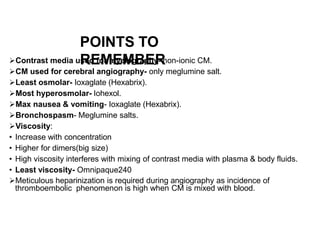
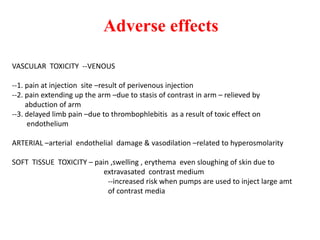
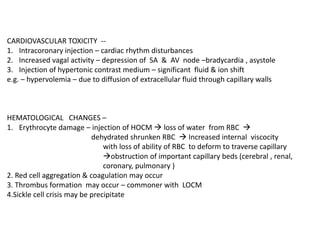
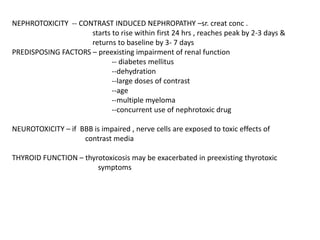
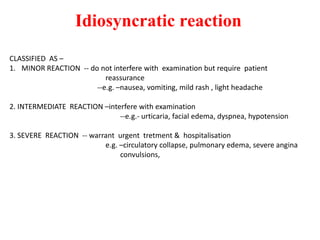
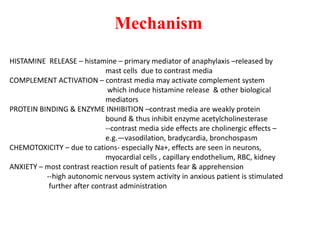
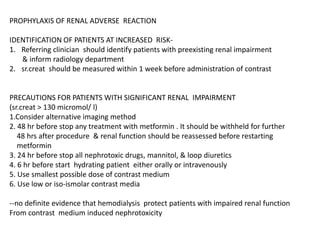
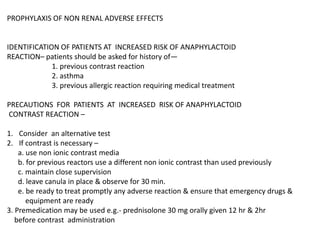
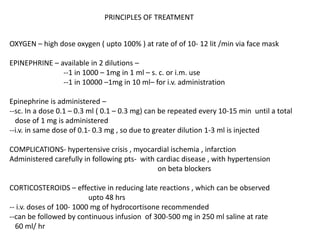
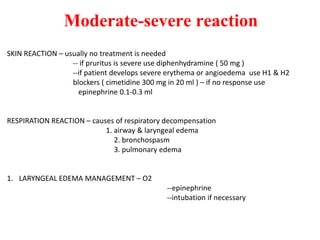
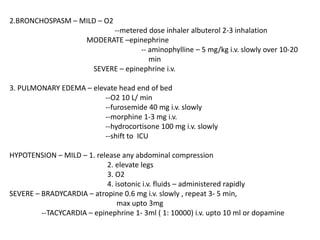
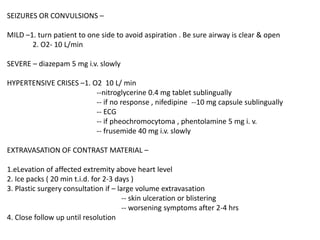
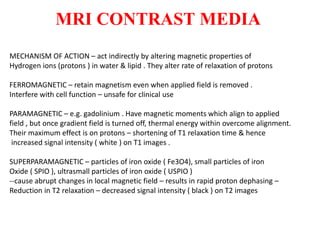
The document discusses contrast agents used in medical imaging, including desirable properties like safety and effectiveness, types such as positive iodine-based and negative air/gas agents, administration methods, and examples of examinations. Adverse effects are outlined for different contrast media based on properties like osmolality and ionicity. The ideal contrast agent is described as having high solubility, stability, biocompatibility, and selective excretion with minimal adverse impacts.