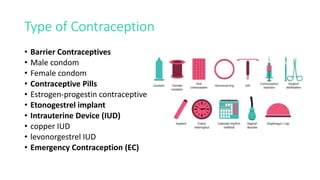
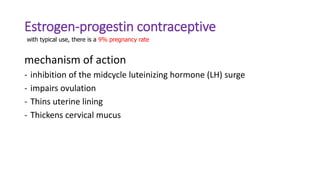
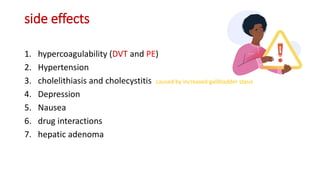
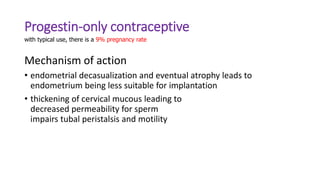
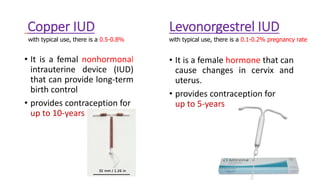
A 24-year old woman presents to her gynecologist concerned about a condom breaking during intercourse two days prior. She is not ready for a child and inquires about emergency contraception. The doctor discusses options including the morning after pill and copper intrauterine device. The woman requests to have a copper IUD inserted as it is the most effective form of emergency contraception and will also provide long-term contraception. The document then outlines and compares various contraception methods including barrier methods, hormonal pills, implants, IUDs, and emergency contraception options.