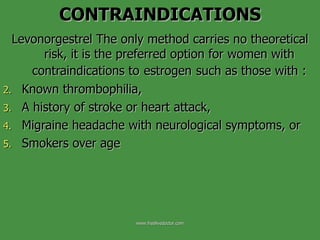
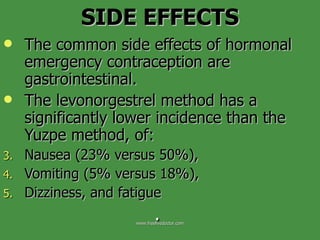
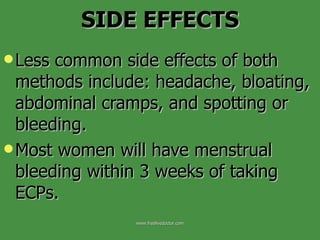
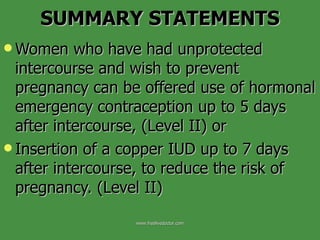
Emergency contraception methods include hormonal emergency contraceptive pills containing levonorgestrel or a combination of levonorgestrel and ethinyl estradiol, or insertion of a copper IUD. Levonorgestrel-only emergency contraception is more effective and has fewer side effects than the Yuzpe method. Emergency contraception is effective in preventing pregnancy when used within 5 days of unprotected intercourse but efficacy declines with increasing time between intercourse and treatment. Providing advance access to emergency contraception does not reduce use of regular contraceptive methods.