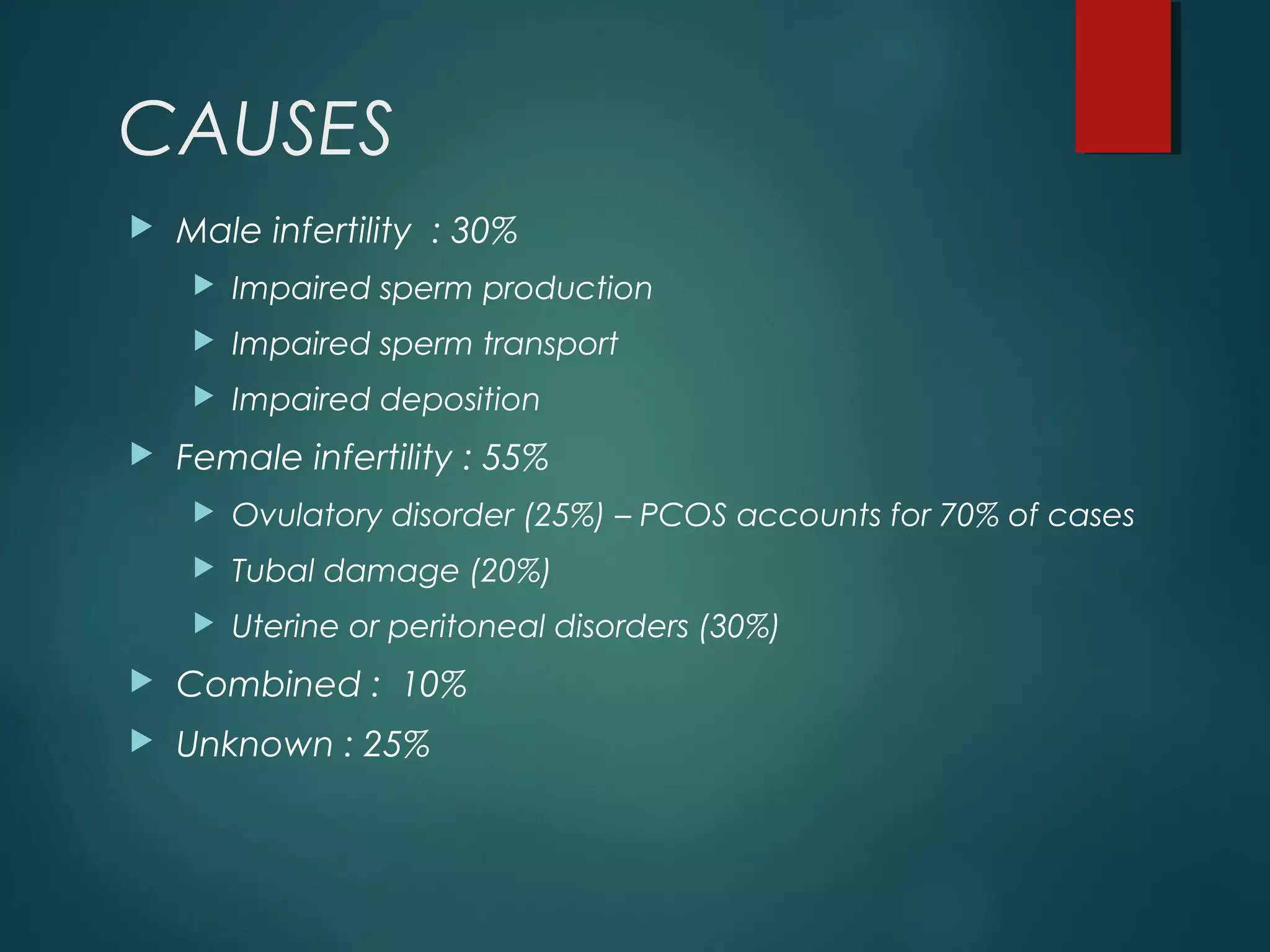
This document provides information on infertility, including its definition, causes, risk factors, diagnosis and investigations, and management options. It defines infertility as not conceiving after one year of unprotected sex. The most common causes are male factors (30%), ovulatory disorders (25%), and tubal damage (20%). Risk factors include advanced age, smoking, alcohol, weight factors, and certain infections or exposures. Diagnosis involves medical history, physical exams, and tests like semen analysis, ovulation assessments, and imaging. Treatment may include lifestyle changes, medications, surgery, and assisted reproductive technologies like IUI, IVF, and ICSI.


![Risk Factors
Age
peak fertility : early of the third decade of life.
beyond 35 years (and particularly after age 40 years), the
likelihood of becoming pregnant is getting less.
Dunson DB, Baird DD, Colombo B [2004]. Increased infertility with age
in men and women. Obstetrics and Gynecology 103: 51–6.](https://image.slidesharecdn.com/infertility-150602070831-lva1-app6891/75/Infertility-5-2048.jpg)