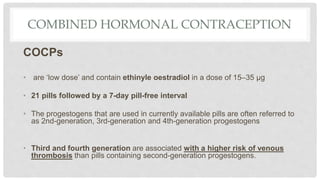
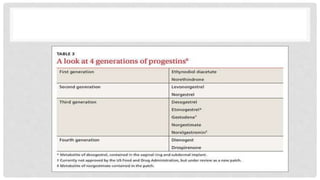
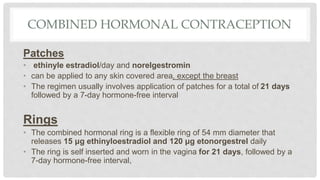
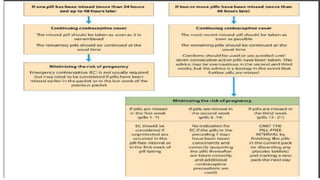
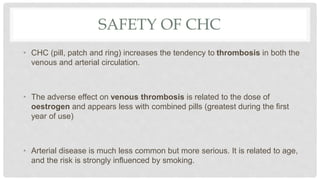
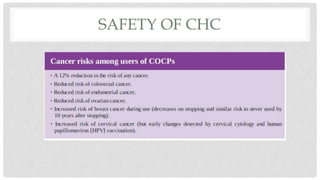
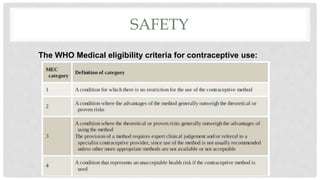
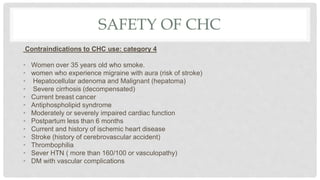
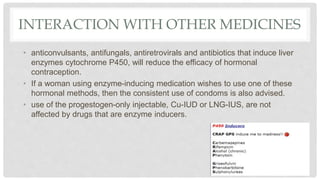
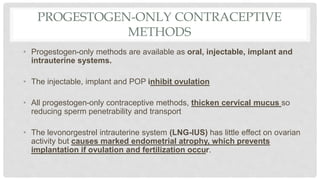
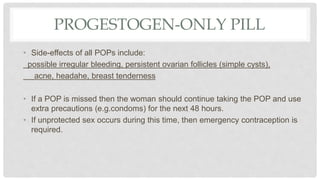
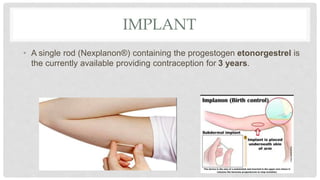
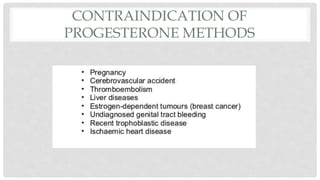
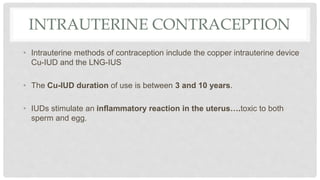
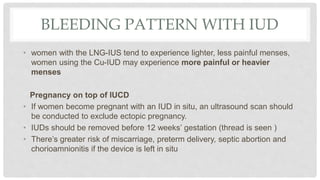
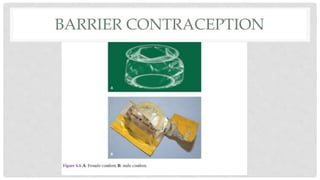
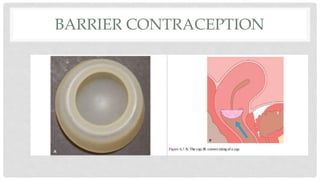
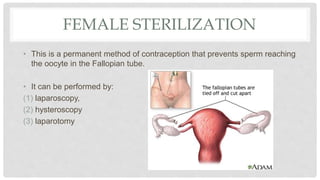
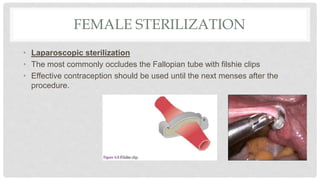
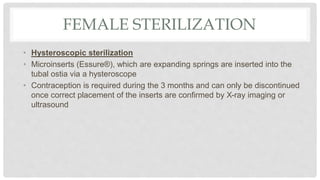
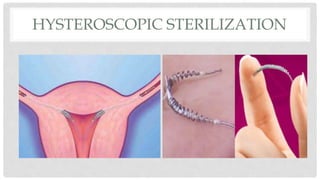
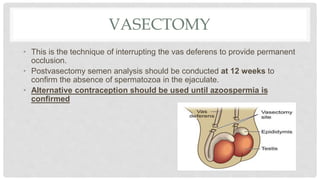
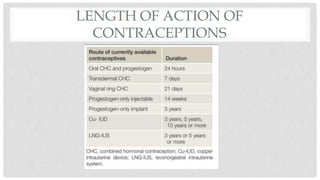
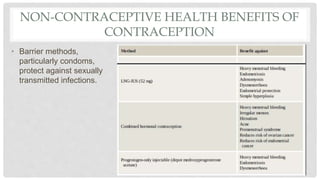
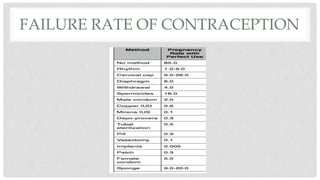
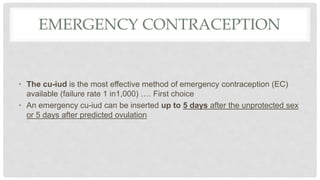
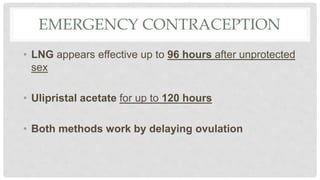
This document discusses various methods of contraception, including hormonal methods like combined oral contraceptives and progestogen-only pills, implants, injections, and IUDs. Barrier methods like condoms and diaphragms are also covered. Long acting and permanent options like IUDs, sterilization procedures, fertility awareness methods, and emergency contraception are summarized. Risks, efficacy, and other details are provided for each method.