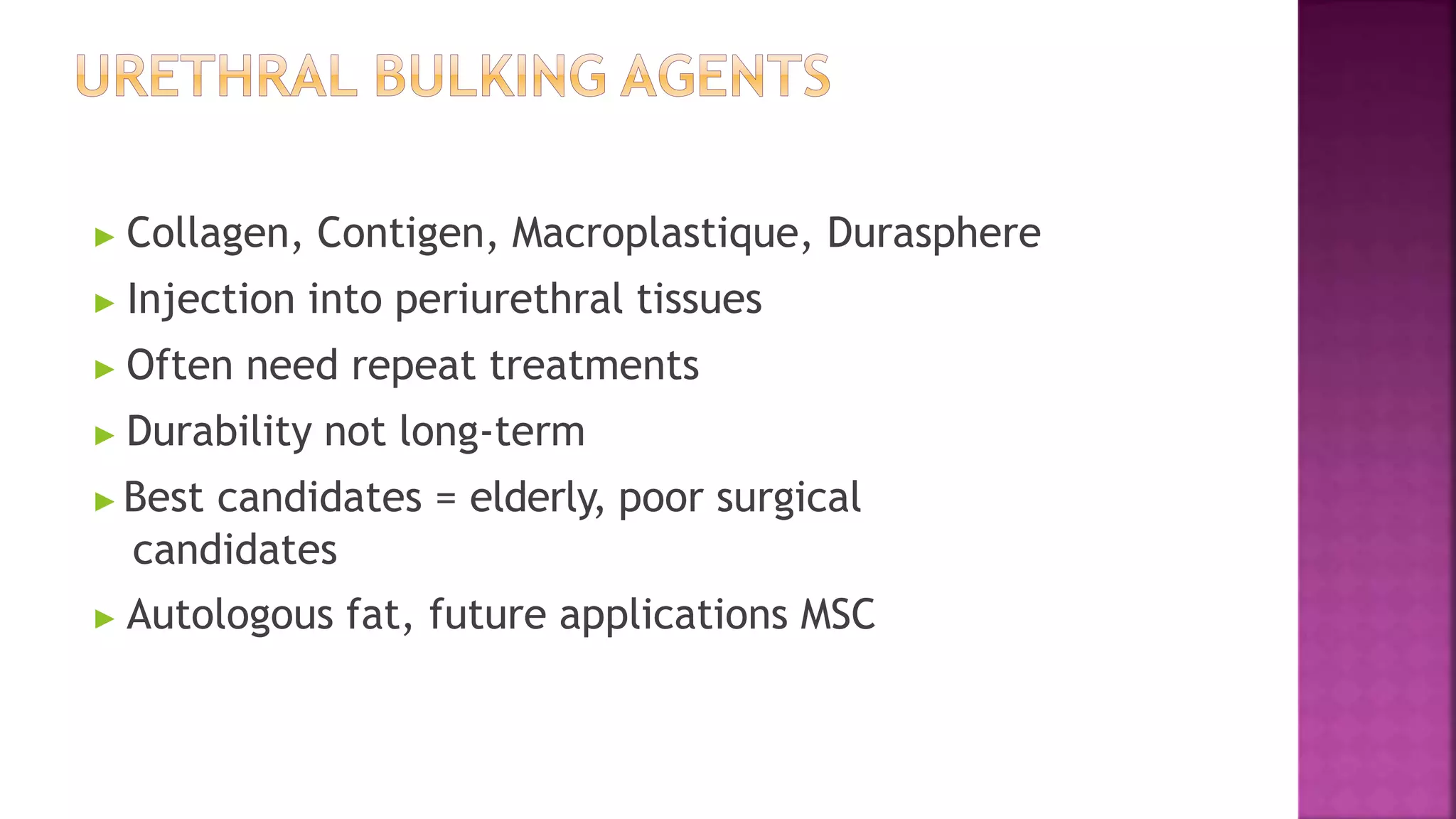
This document discusses urinary incontinence and pelvic organ prolapse. It begins by outlining the objectives and prevalence of these conditions, which commonly affect women. It then describes the different types of urinary incontinence and treatments available, including both surgical and non-surgical options. The document also discusses pelvic organ prolapse, including causes, symptoms, assessment methods, and treatment approaches. Overall, it provides an overview of these common conditions and reviews evaluation and management strategies.