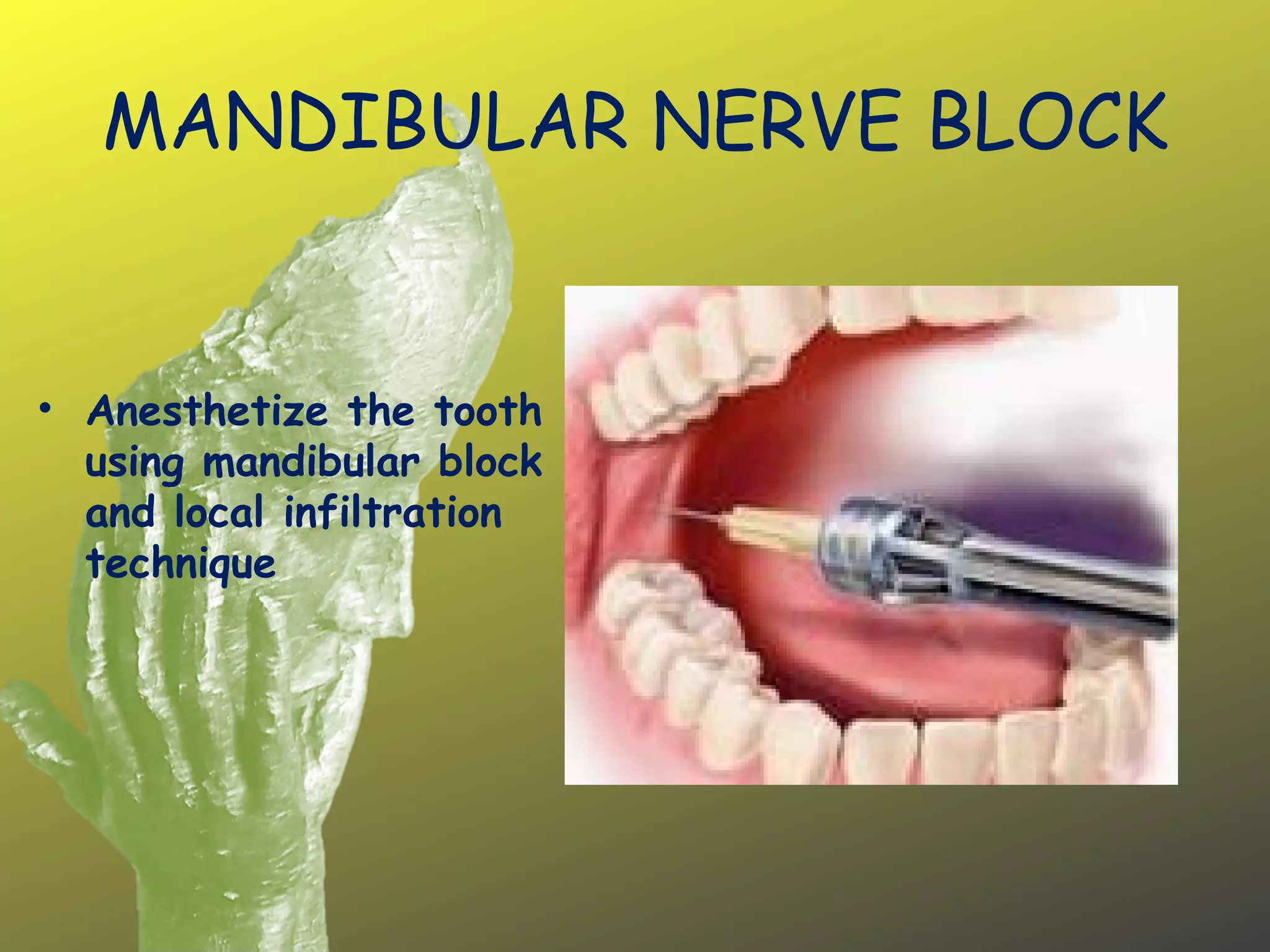
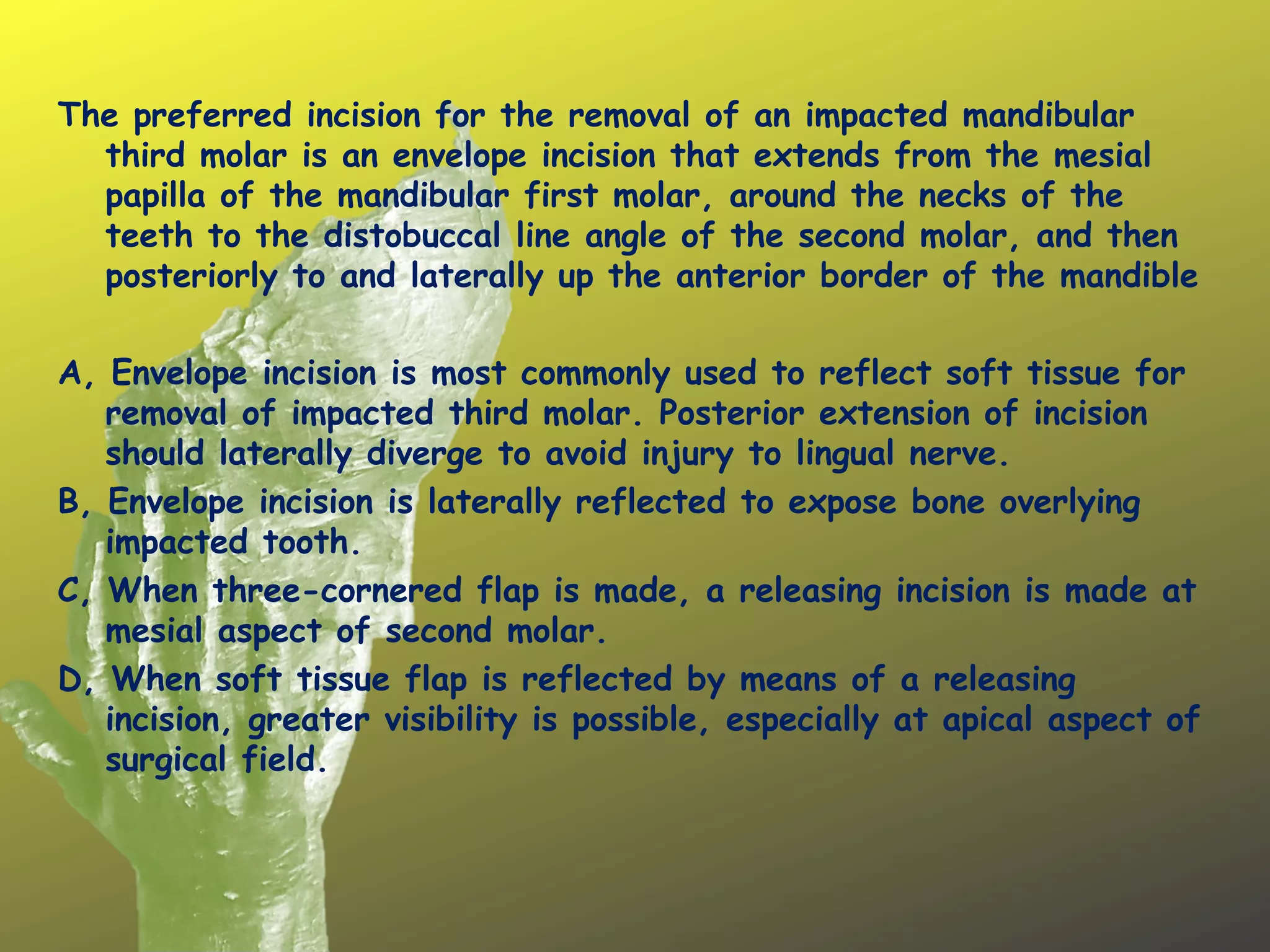
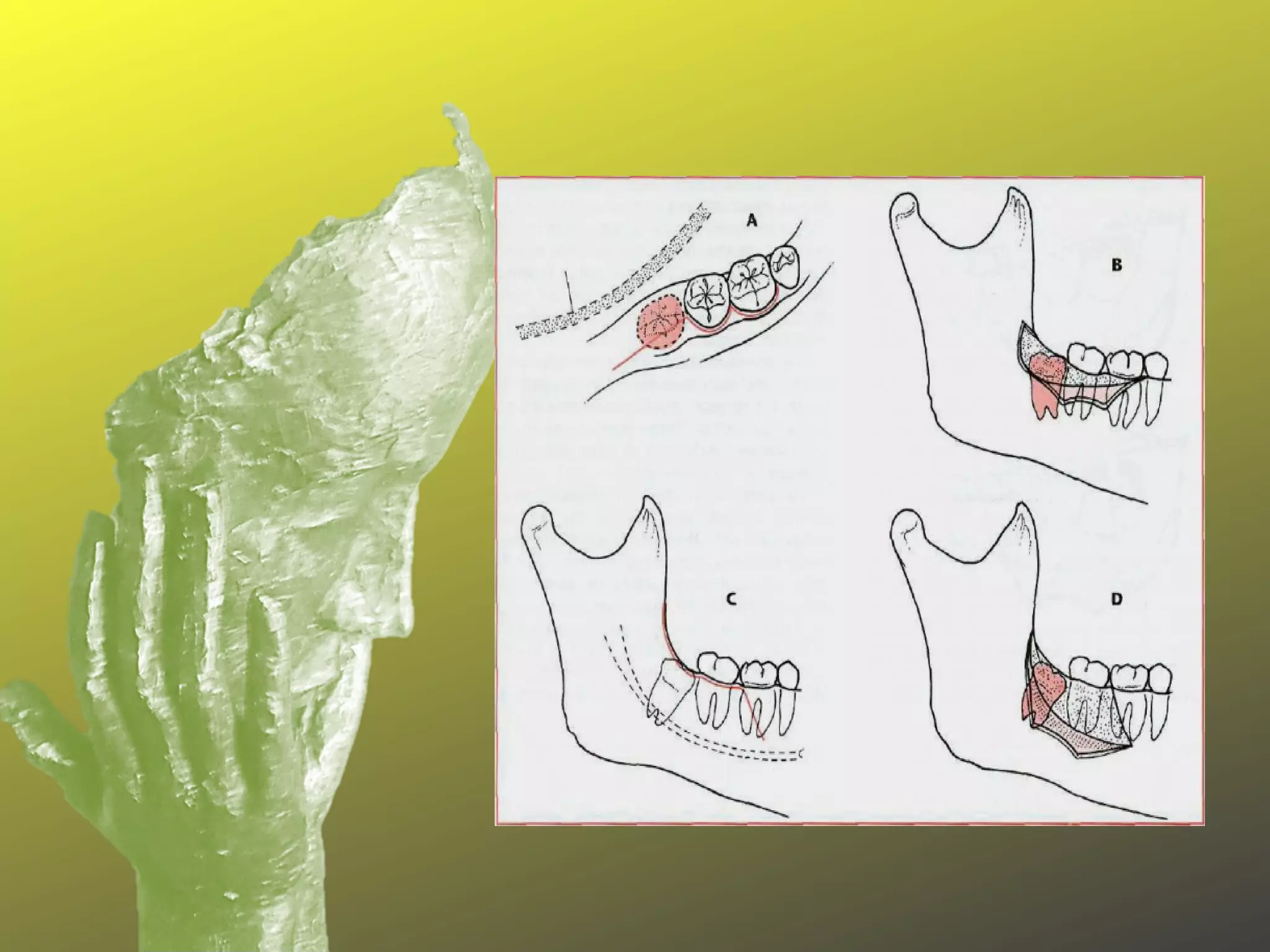
(1) This document describes the procedure for removing an impacted mandibular third molar tooth, known as an odontectomy. (2) The procedure involves making an envelope incision, reflecting the soft tissue flap, removing overlying bone, sectioning and extracting the tooth with elevators, curreting the socket, and placing sutures. (3) Post-operative instructions are provided which include taking antibiotics and pain medications, applying ice, avoiding smoking and spicy foods, and following up with the dentist after 1 week.