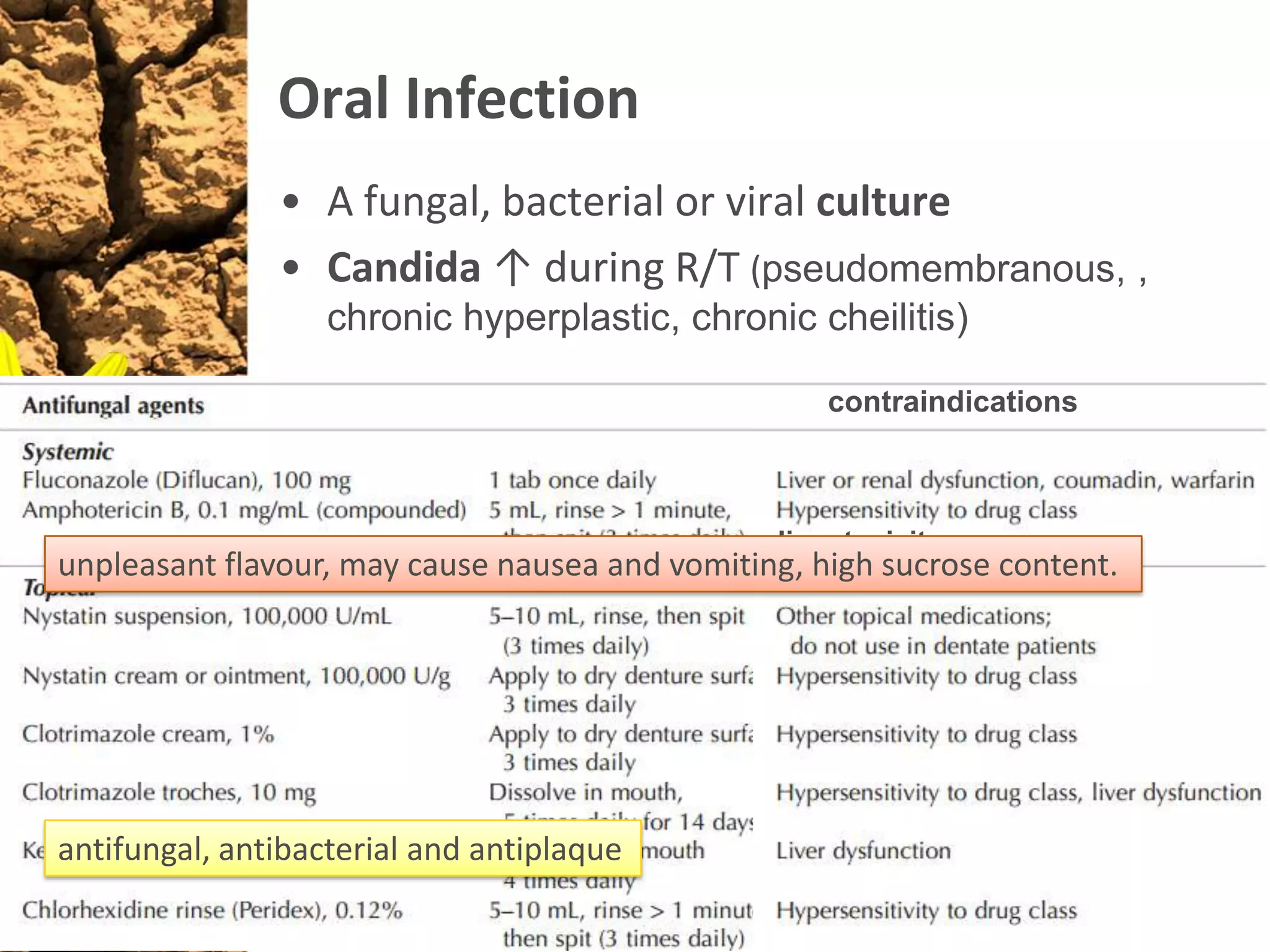
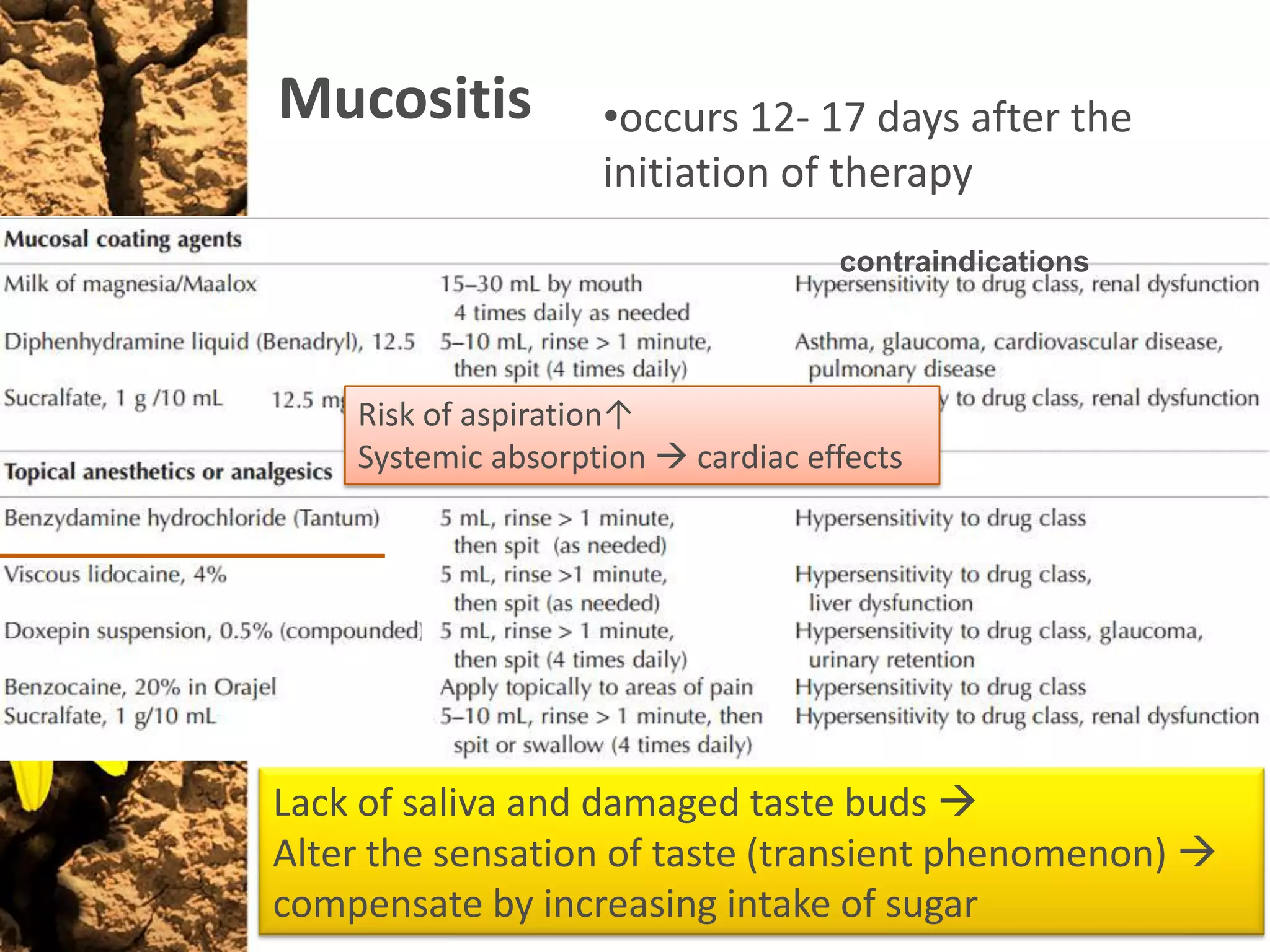
The document summarizes guidelines for oral assessment and management before, during, and after head and neck radiation therapy (R/T). It recommends a complete dental examination before R/T to identify issues and extractions to reduce complications. During R/T, daily oral hygiene and topical fluoride are emphasized to prevent side effects like mucositis, infection, and xerostomia. Long-term, frequent follow-up is needed due to risks like osteoradionecrosis and new malignant disease. The goal is to minimize oral morbidity at all treatment stages.