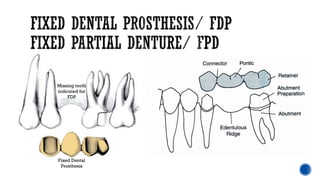
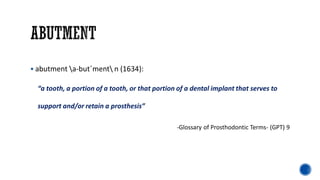
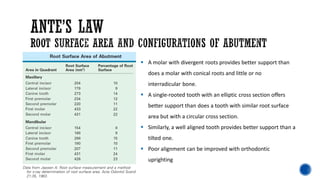
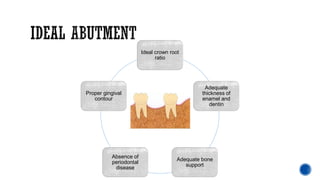
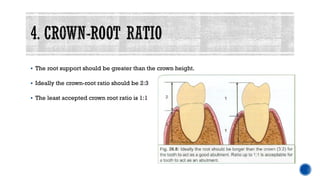
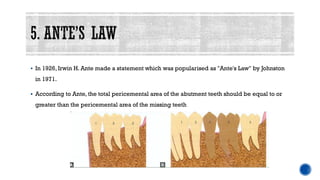
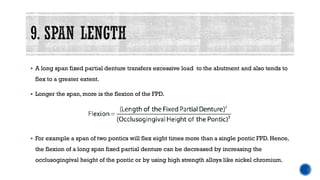
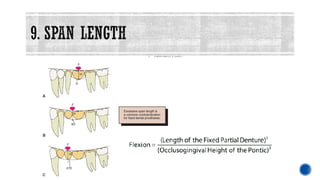
This document discusses factors to consider when selecting abutment teeth for fixed partial dentures. It outlines Ante's law which states the root surface area of abutment teeth should be greater than or equal to the teeth being replaced. Ideal abutments have adequate root length and bone support, proper crown-root ratio, and good periodontal health. Other considerations include a patient's occlusion, arch form, oral health, and long-term prognosis of the abutment teeth. Careful evaluation of anatomical, functional and biological factors is necessary for successful abutment selection and long-term outcomes.