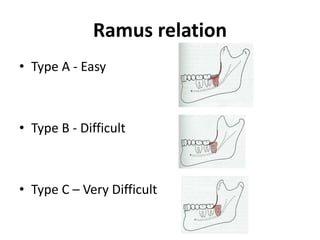
The document provides an overview of mandibular impacted 3rd molar removal, including indications for removal, factors to assess difficulty, the surgical procedure, potential complications, and post-operative care. Key areas of assessment that influence difficulty include depth of impaction, angulation, proximity to important structures like the inferior dental nerve. Thorough pre-operative evaluation and careful technique during removal can help reduce risks of complications.