The document provides a comprehensive overview of meniscal injuries, including anatomy, types of tears, etiology, clinical features, management, and recent advances in treatment. It highlights that meniscal injuries are prevalent, particularly among athletes, and categorizes tears into various types including radial, vertical, and chronic tears, each with distinct characteristics and management approaches. Furthermore, it discusses the details of both conservative and surgical rehabilitation methods required for recovery post-injury.





























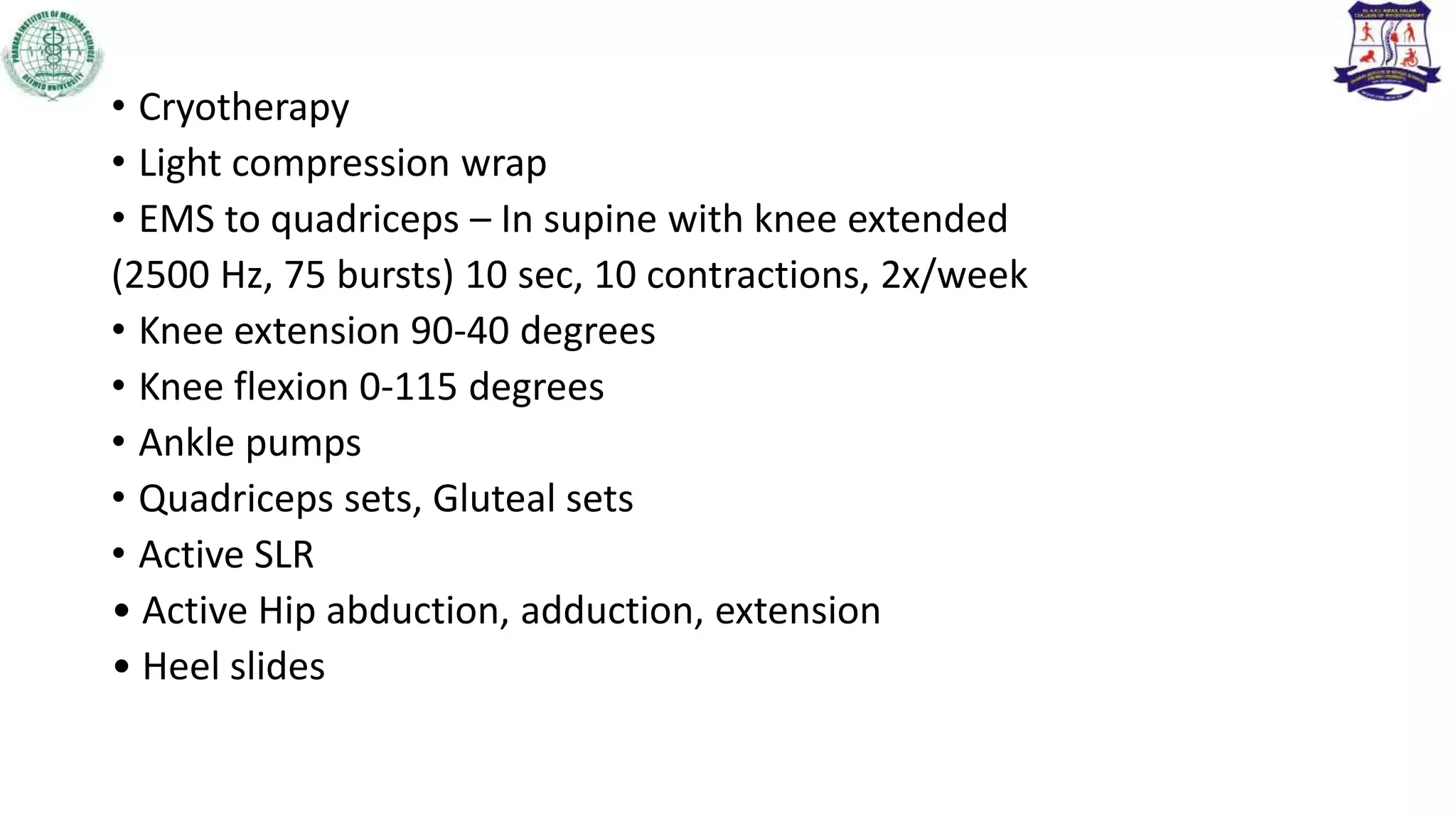
![Subacute phase (up to 3 weeks)
Promote healing of injured tissues
• Monitor response of tissue to exercise progression; decrease intensity
if inflammation increases.
• Protect healing tissue with assistive devices, splints, tape, or wrap;
• progressively increase amount of time the joint is free to move each
day and decrease use of assistive device as strength in supporting
muscles increases.
Note :- [Weight bearing considerations : Partial weight bearing within
the tolerance of the healing tissues may be used]](https://image.slidesharecdn.com/meniscalinjury-230501045037-1f25cb88/75/Meniscal-injuries-and-physiotherapy-management-35-2048.jpg)