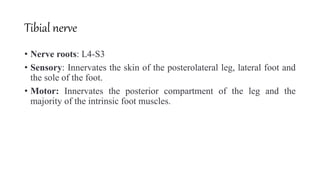
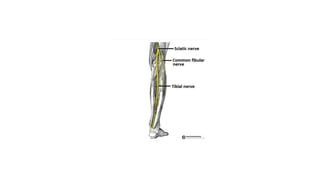
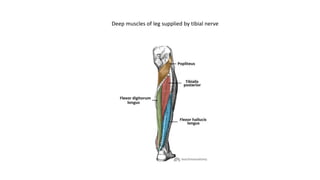
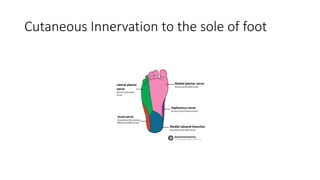
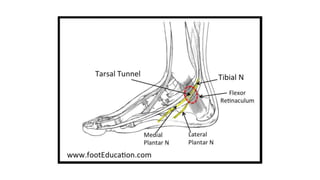
The document discusses peripheral nerve injuries, specifically the tibial and peroneal nerves, detailing their anatomical functions, clinical implications of injuries, diagnostic methods, and treatment options. It highlights conditions such as tarsal tunnel syndrome and common peroneal neuropathy, including their causes, risk factors, symptoms, and differential diagnoses. A comprehensive approach involving history, physical examination, and imaging studies is emphasized for accurate diagnosis and evaluation.