The document discusses various pediatric gastrointestinal disorders including:
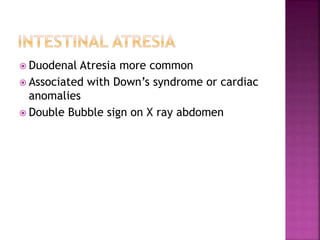
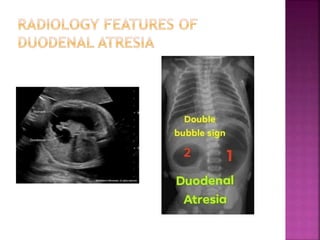
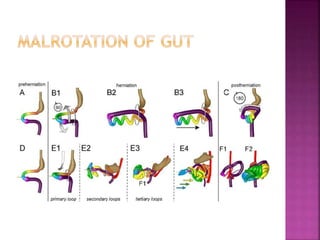
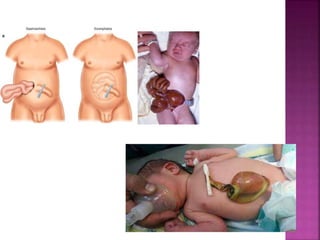
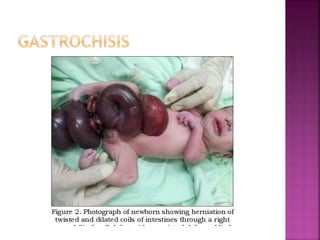
1. Duodenal atresia, malrotation with midgut volvulus, jejunal/ileal atresia as causes of intestinal obstruction.
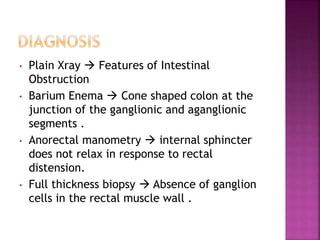
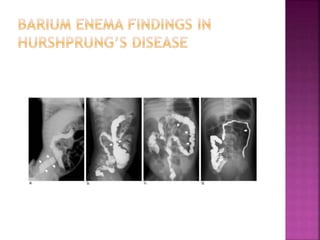
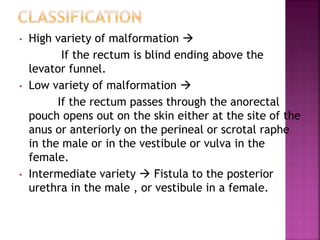
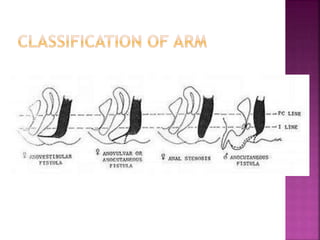
2. Hirschsprung's disease, anorectal malformations, meconium ileus as other causes.
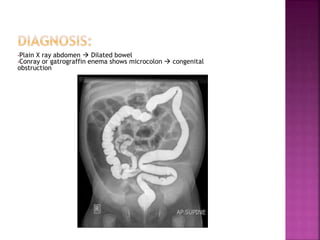
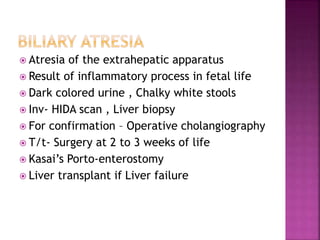
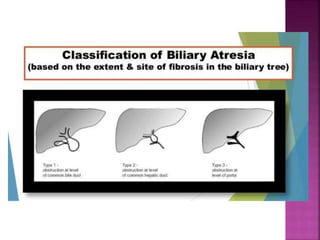
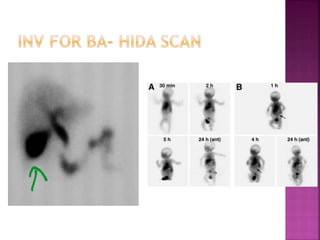
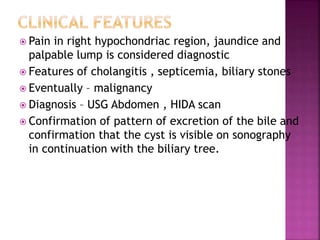
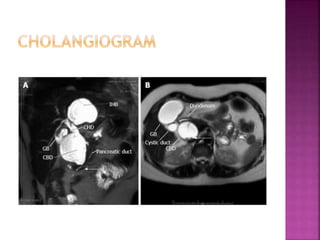
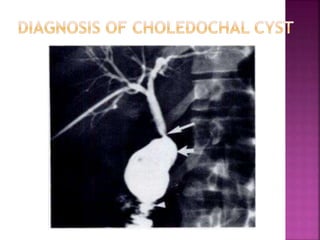
3. Signs, investigations, and management are described for different conditions like biliary atresia.