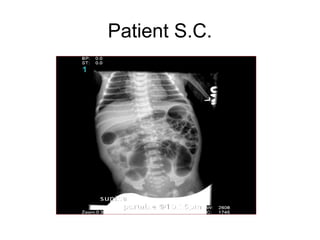
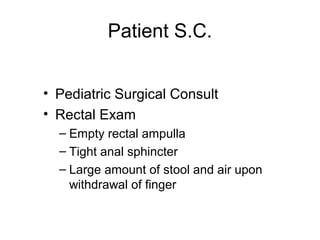
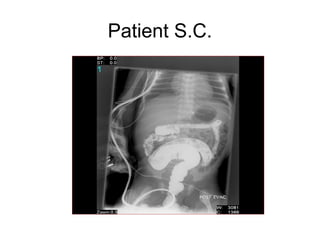
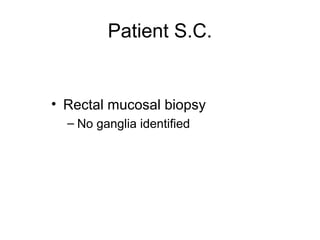
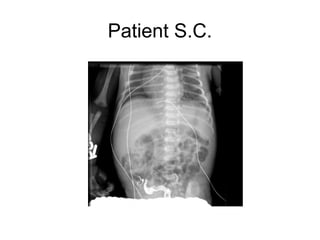
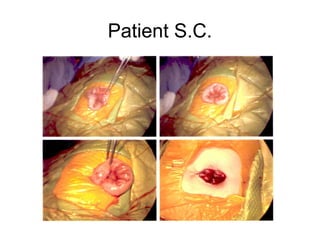
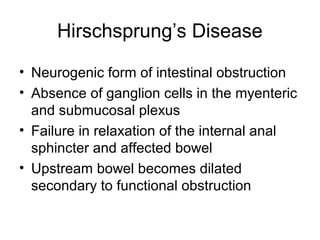
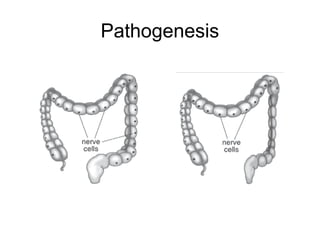
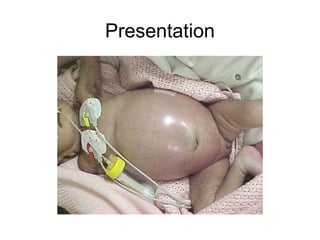
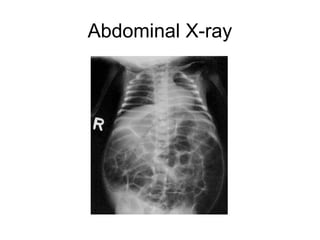
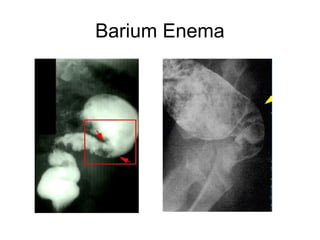
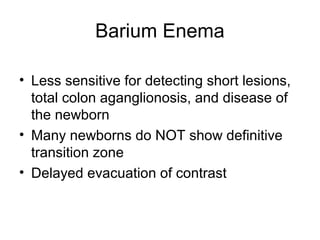
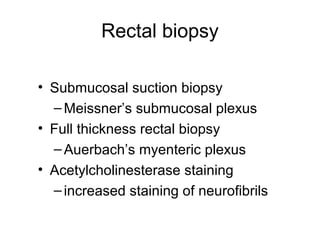
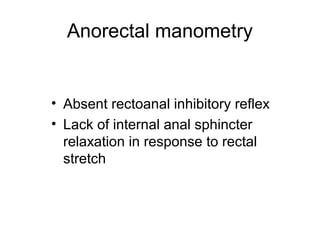
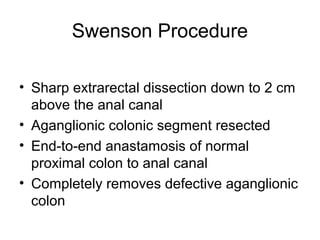
This document discusses the case of a newborn male patient presenting with symptoms of Hirschsprung's disease including abdominal distention and failure to pass meconium. Diagnostic testing revealed the absence of ganglion cells in the colon consistent with Hirschsprung's disease. The patient underwent an end colostomy and biopsy which confirmed the diagnosis. He recovered well and was discharged with plans for a future pull through surgery.