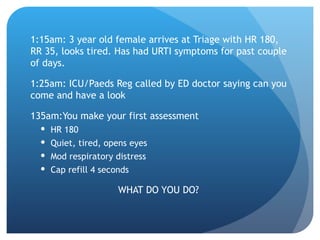
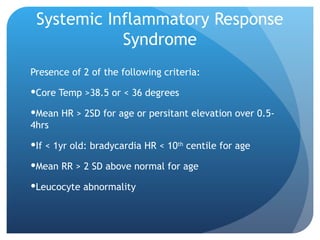
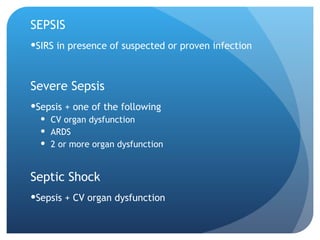
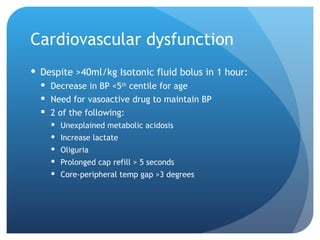
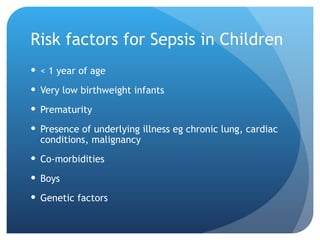
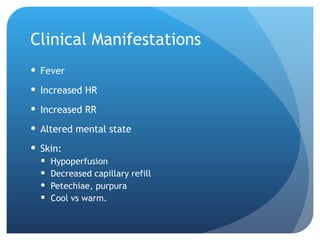
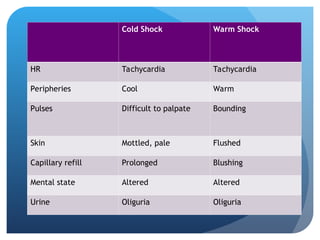
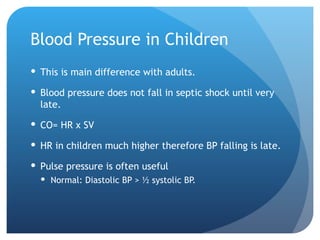
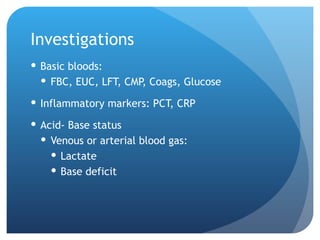
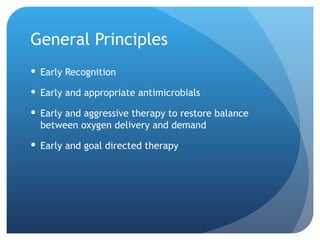
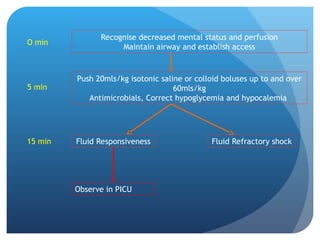
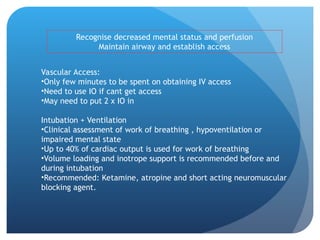
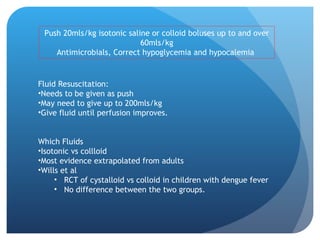
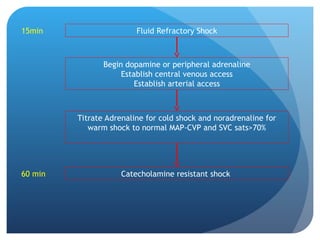
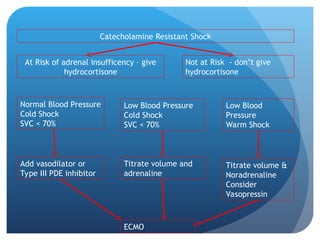
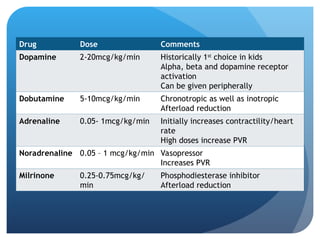
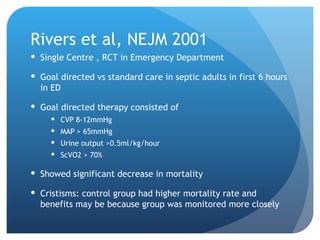
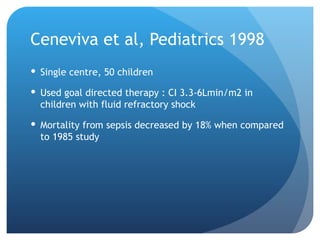
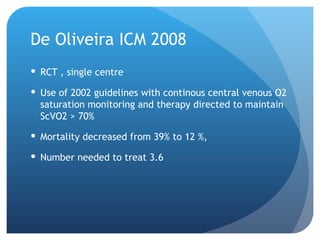
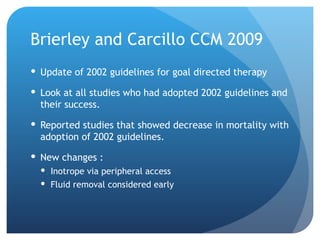
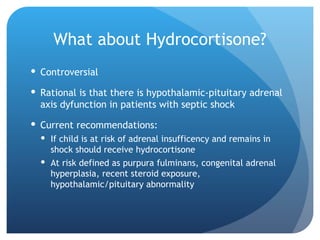
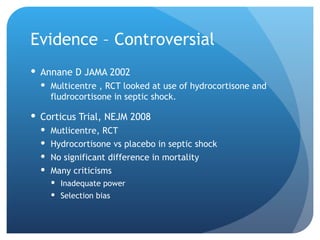
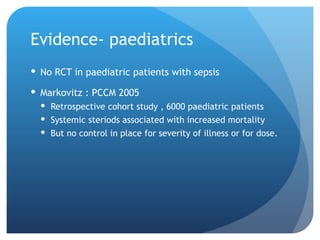
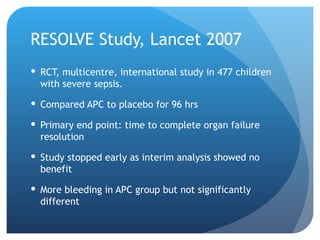
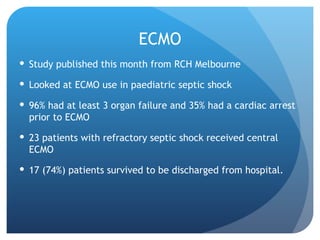
The document outlines the assessment and management of pediatric septic shock, highlighting the critical need for early recognition and timely intervention to reduce mortality risks, which can be as high as 30%. It discusses definitions, clinical manifestations, risk factors, and the importance of aggressive fluid resuscitation and antimicrobial therapy, as well as treatment protocols involving vasoactive drugs. The document emphasizes the significance of goal-directed therapy in improving outcomes and discusses controversies surrounding the use of hydrocortisone and other therapeutic measures.