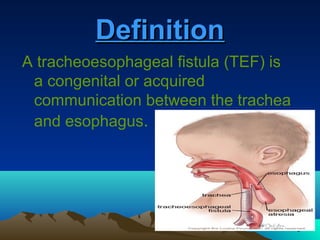
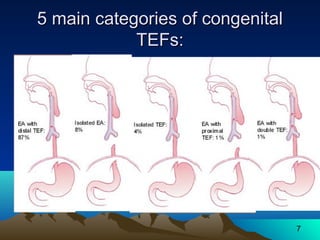
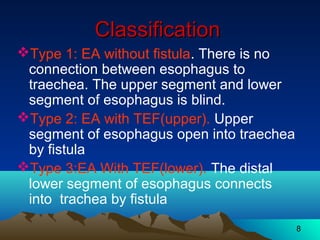
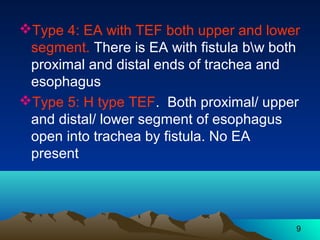
1) Tracheoesophageal fistula (TEF) is a congenital abnormality where the trachea and esophagus are connected by an abnormal passageway. There are different types depending on the location of the fistula.
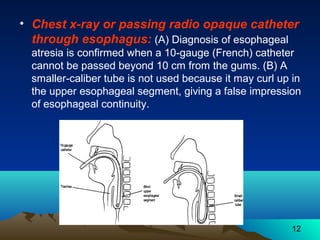
2) Clinical manifestations include excessive salivation, coughing or choking with feeds, and respiratory distress. Diagnosis involves imaging studies and endoscopy to locate the fistula.
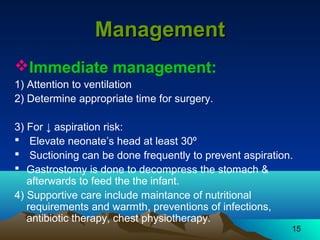
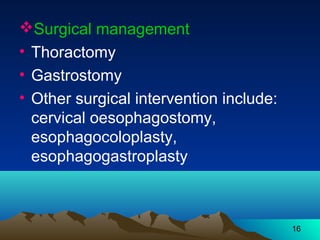
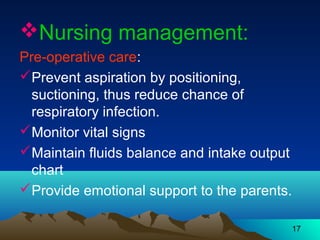
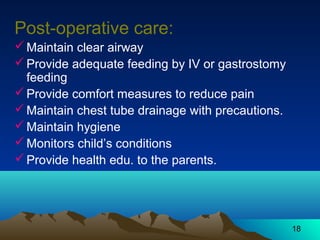
3) Surgical repair is usually required to separate the trachea and esophagus. Post-operative nursing care focuses on maintaining airway patency, feeding via gastrostomy tube, and preventing infections.