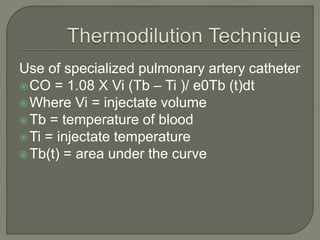
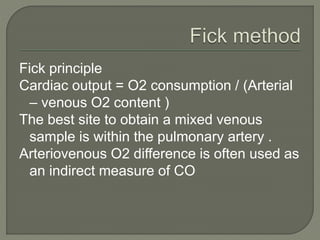
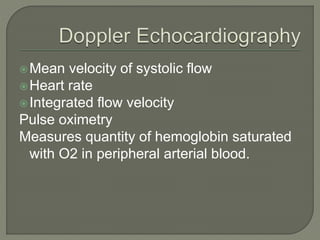
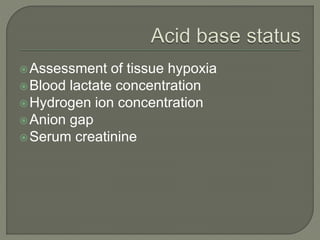
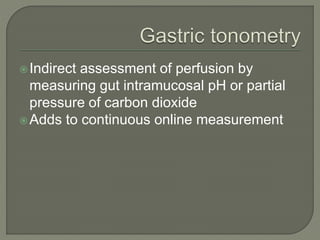
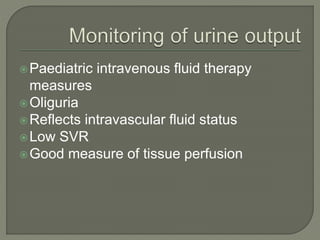
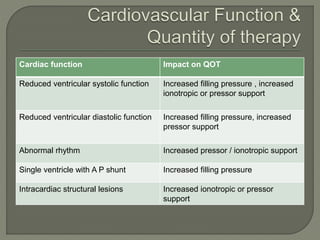
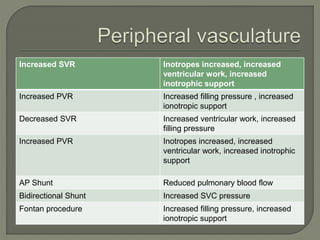
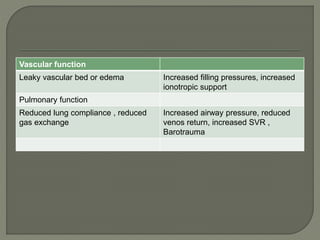
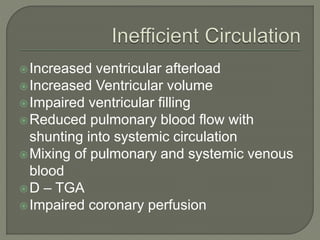
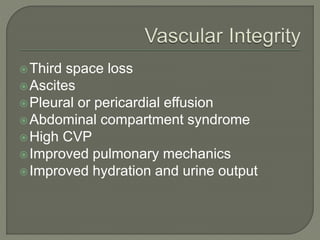
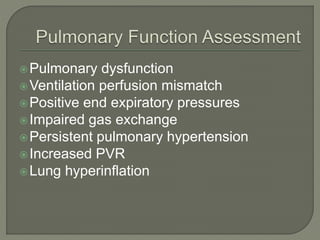
The document outlines various cardiovascular assessment and monitoring techniques in pediatric intensive care units, emphasizing the importance of physical examination, diagnostic imaging, and blood pressure monitoring. It discusses key indicators of cardiac function such as heart rate, blood flow, and oxygen transport, and details methods for evaluating tissue hypoxia and intravascular fluid status. The document also covers implications of cardiac function on patient management, including the use of inotropes and the impact of pulmonary and vascular health on overall patient outcomes.