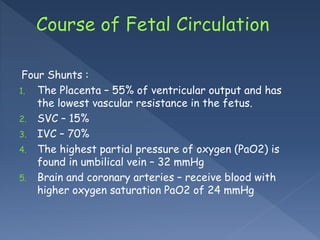
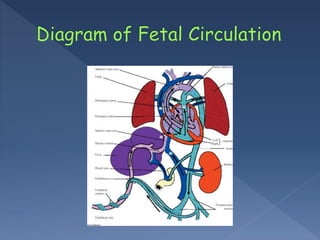
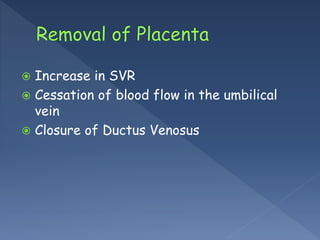
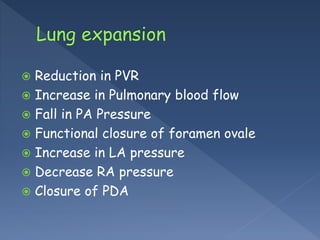
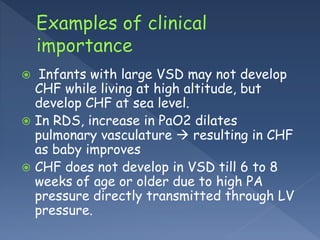
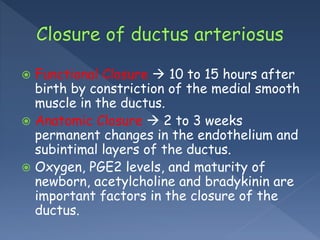
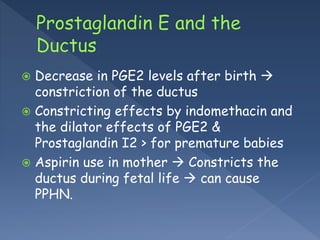
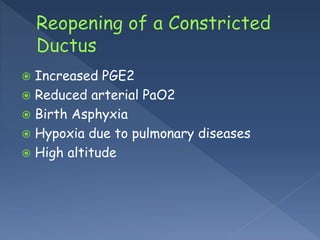
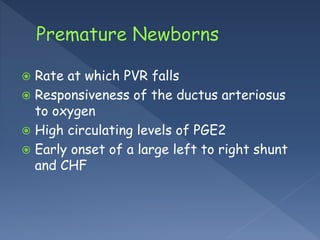
The document discusses the fetal circulatory system, highlighting the role of the placenta and various shunts in blood flow and oxygen exchange. It also covers the transition to postnatal circulation, including the closure of the ductus venosus and changes in pulmonary blood flow, and factors affecting the ductus arteriosus. Additionally, it notes the implications of pulmonary conditions and high altitude on circulation and potential heart failure in infants.