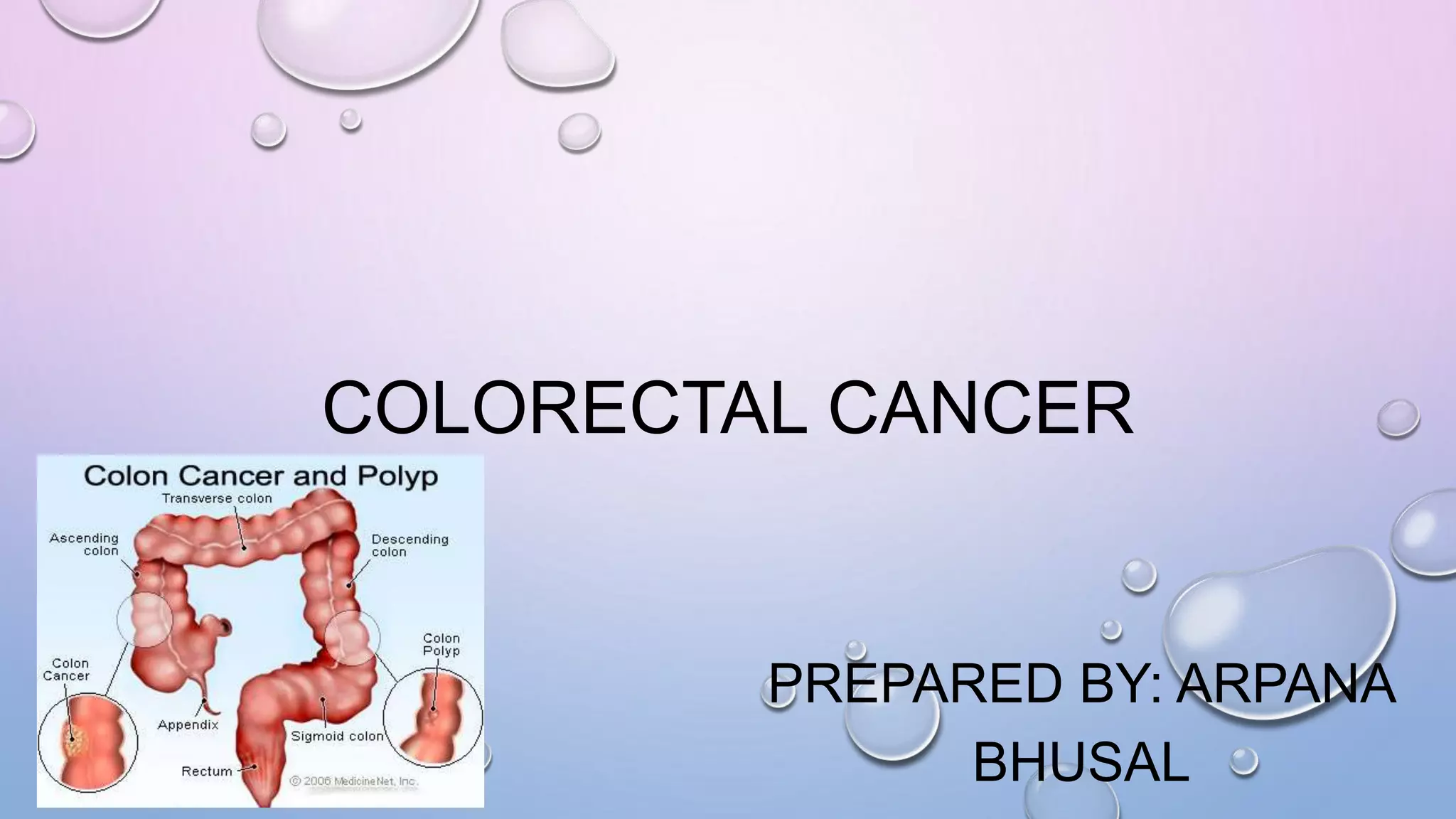
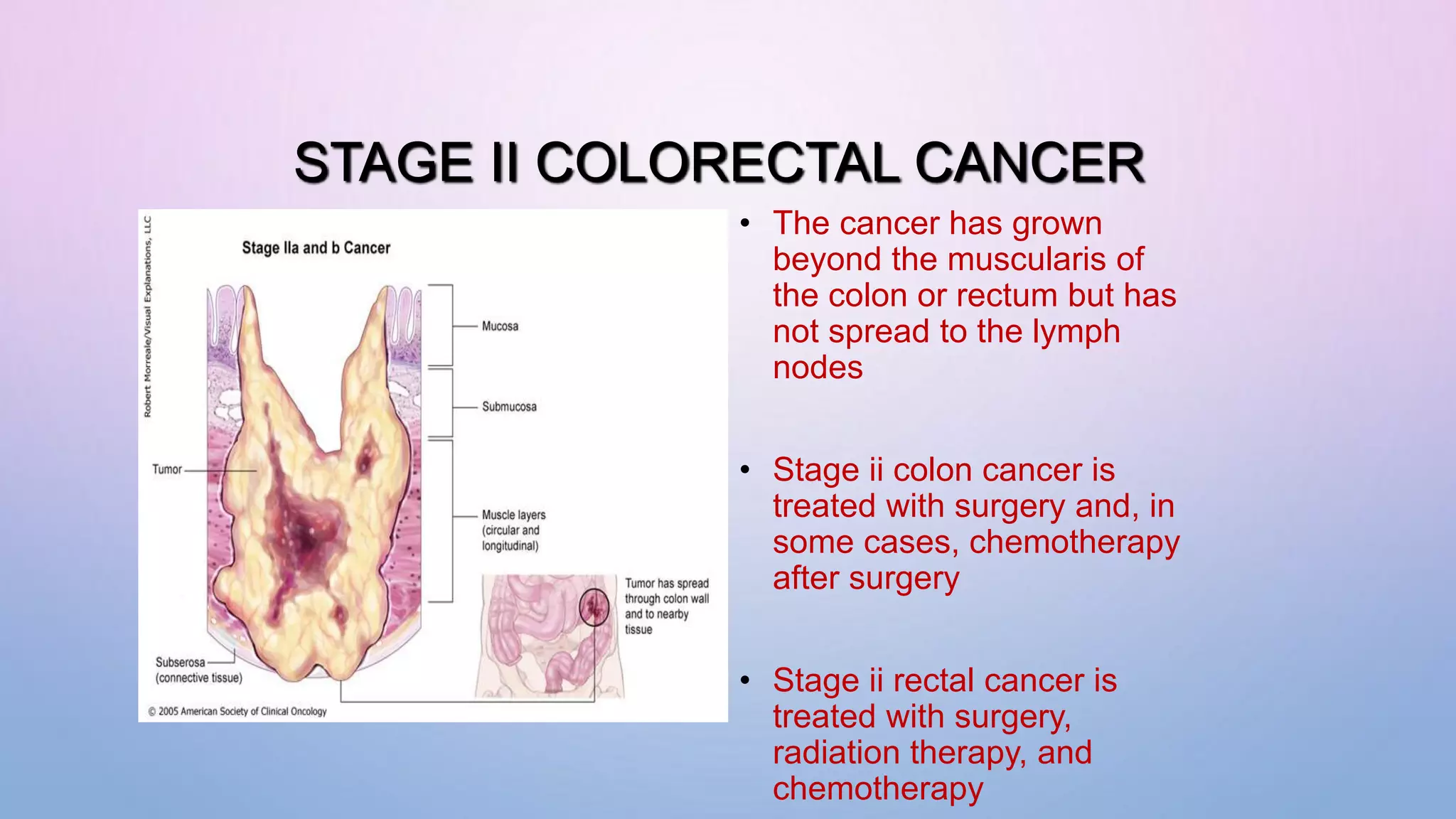
Colorectal cancer is the third most common cancer and second leading cause of cancer death. It begins as a noncancerous polyp that over time can become cancerous. Risk factors include polyps, age, inflammatory bowel disease, diet high in red meat, family history, obesity, smoking, and alcohol. Genetic and environmental factors both contribute to development. Screening is recommended for those over 50 or those with family history. Treatment depends on stage - early stage is often surgery while later stages involve chemotherapy, radiation, and surgery. Goals are to remove cancer, kill remaining cells, and prevent return in early stages or slow growth and manage symptoms in advanced cancer.