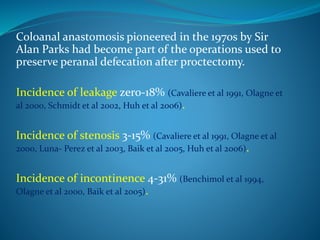
This document discusses coloanal anastomosis (CAA), which has been used since the 1970s to preserve bowel control after rectal resection surgery. The author analyzes data from 13 patients who underwent CAA at Ain Shams University hospitals from 2008-2011. Complications included anastomotic leakage in 1 patient, stenosis in 2 patients, and mild to moderate incontinence in 3 patients. The author concludes that CAA is a feasible technique that provides good functional outcomes and an acceptable risk of complications. Training in hand sewn CAA is important for younger colorectal surgeons in case stapled anastomosis cannot be performed due to issues like fibrosis or a narrow pelvis.