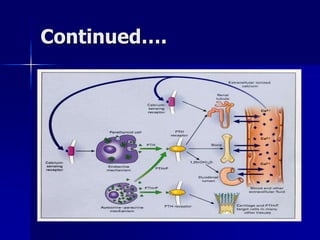
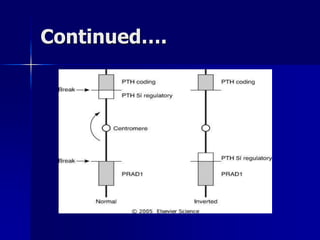
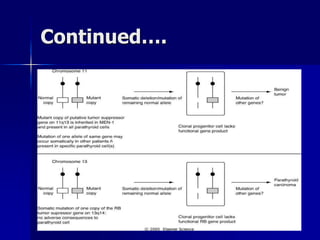
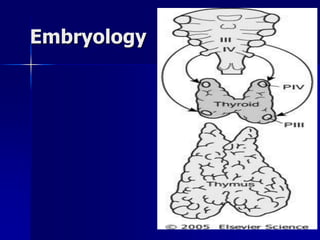
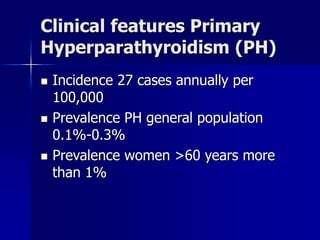
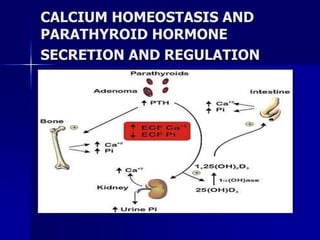
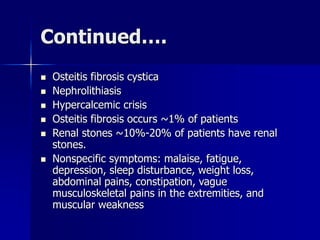
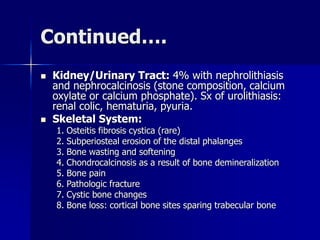
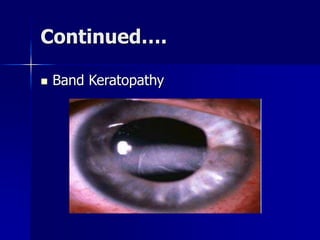
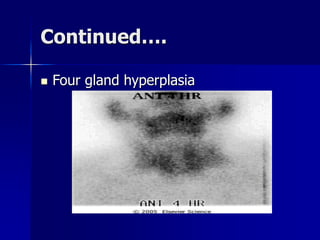
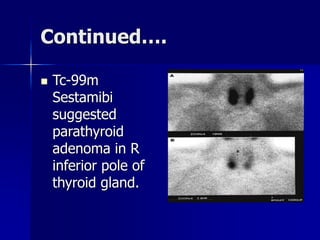
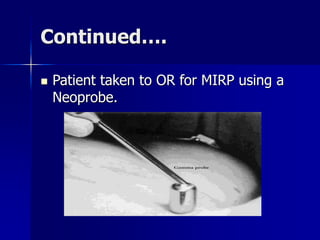
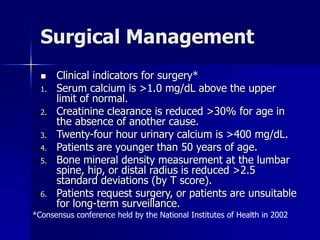
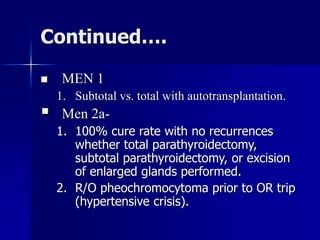
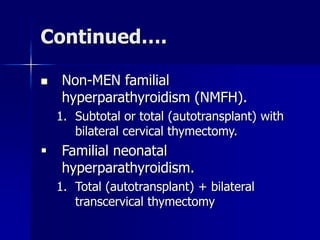
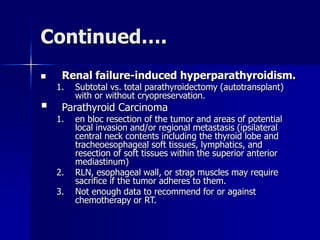
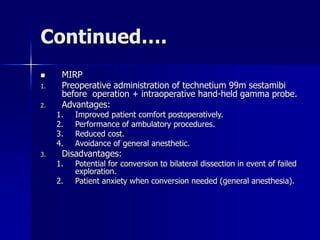
This document discusses the diagnosis and management of parathyroid disease. It begins by reviewing calcium homeostasis and the role of parathyroid hormone. It then covers parathyroid anatomy, histopathology, and embryology. The clinical features, diagnosis, and surgical or medical management of hyperparathyroidism are examined. Localization studies and the molecular basis of these studies are also reviewed. Surgical techniques including minimally invasive parathyroidectomy are discussed. The document concludes by emphasizing the importance of surgical anatomy and embryology for properly diagnosing and treating parathyroid disorders.