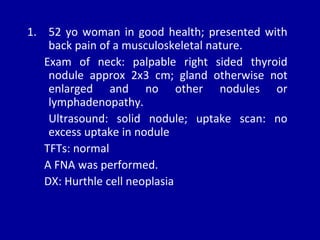
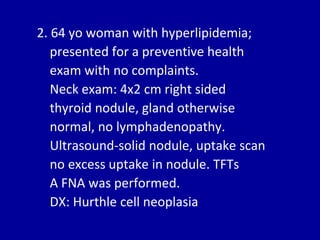
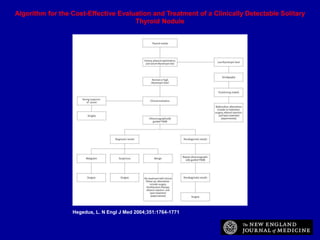
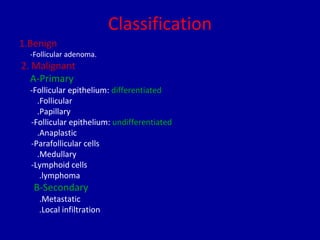
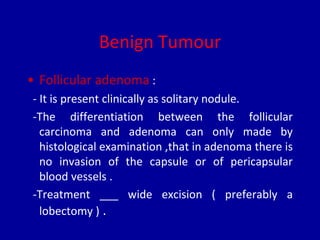
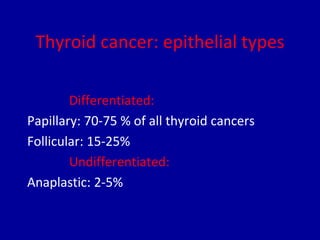
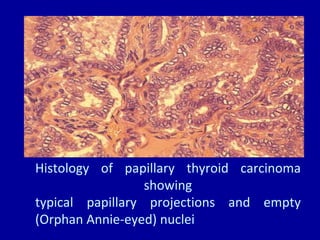
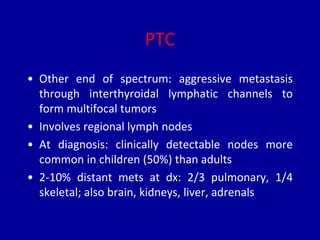
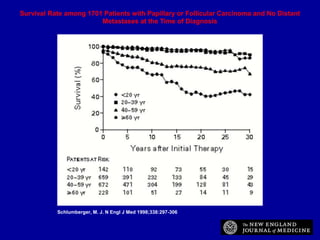
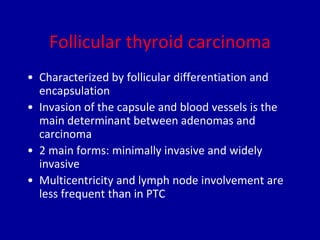
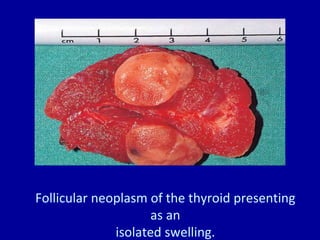
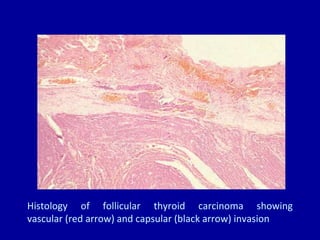
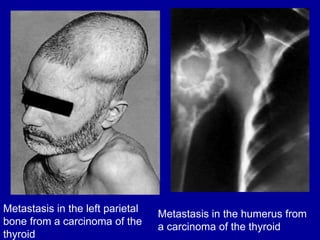
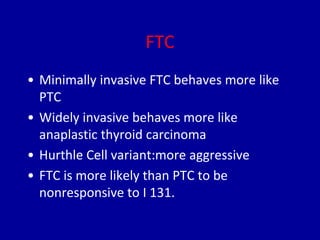
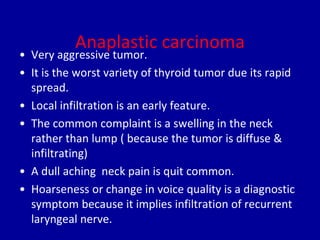
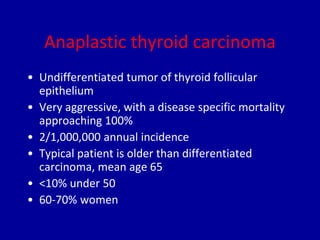
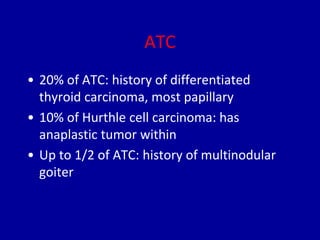
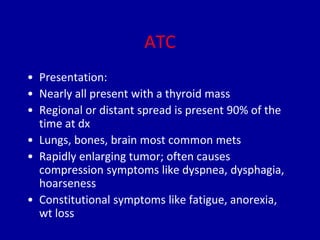
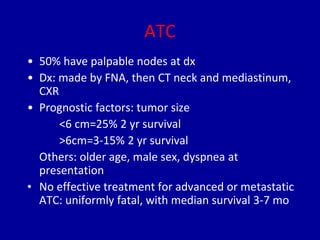
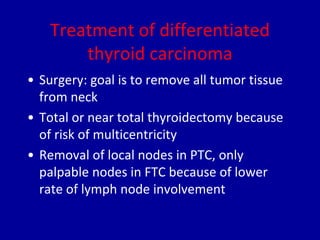
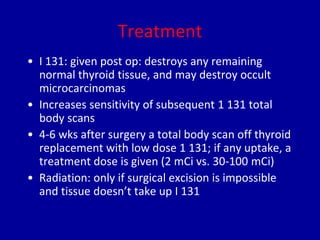
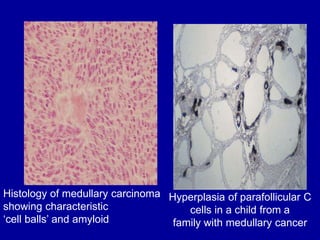
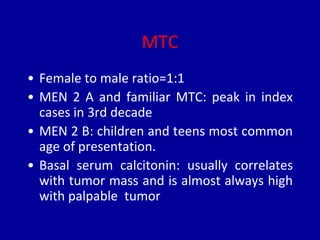
The document summarizes different types of thyroid cancer. It describes three case studies of patients presenting with thyroid nodules who received fine needle aspirations revealing Hurthle cell neoplasia in two cases and papillary thyroid carcinoma in one case. It then discusses the epidemiology, risk factors, classification, clinical characteristics, pathology, treatment and prognosis of the main types of thyroid cancer including papillary, follicular, medullary and anaplastic carcinomas.