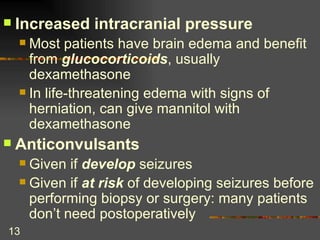
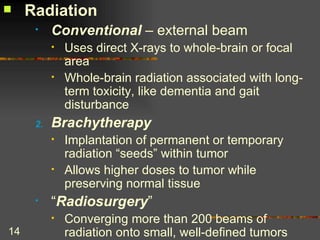
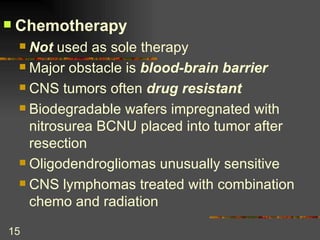
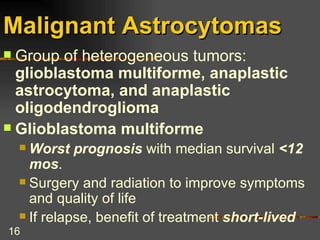
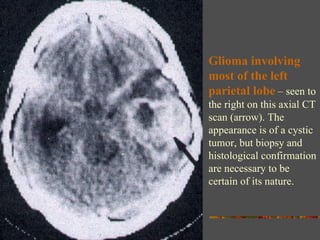
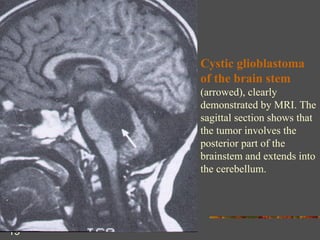
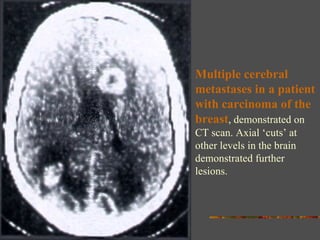
CNS tumors can have devastating effects and high mortality rates. Malignant tumors are difficult to treat if they cannot be completely removed. Primary brain tumors are most commonly from cells of neuroepithelial origin and gliomas arising from astrocytes are the most common. Symptoms depend on the location of the tumor and whether it is primary or metastatic. Treatment involves surgery, radiation, chemotherapy and managing increased intracranial pressure depending on the specific tumor type. Prognosis depends on tumor histology, location and ability to fully resect.