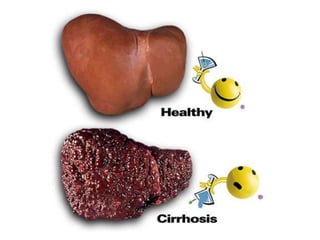
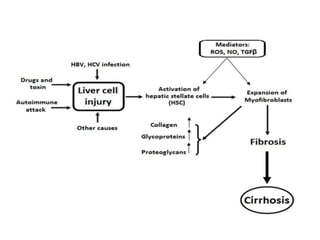
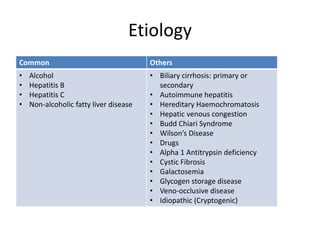
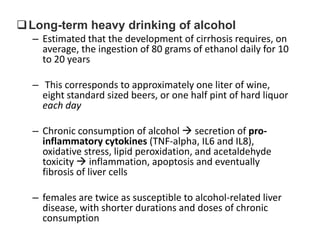
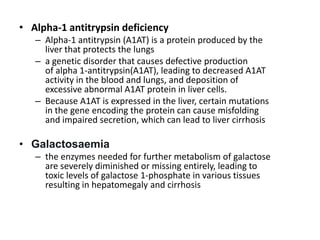
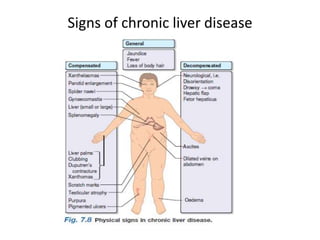
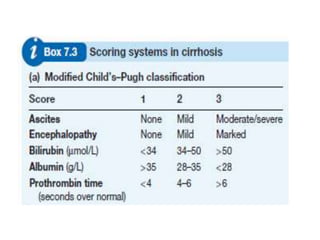
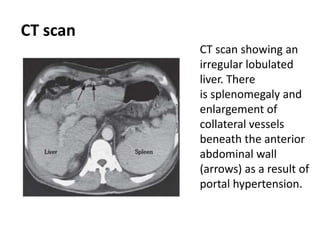
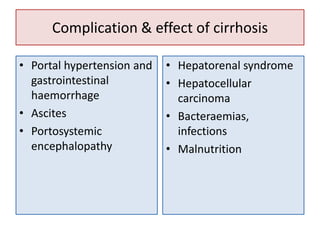
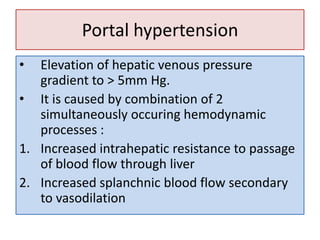
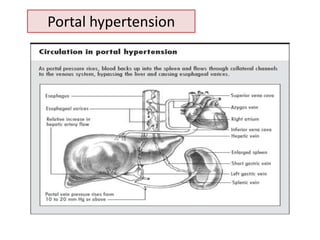
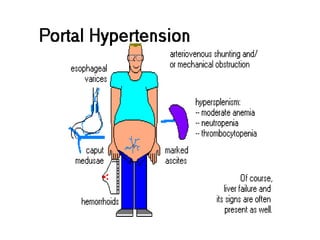
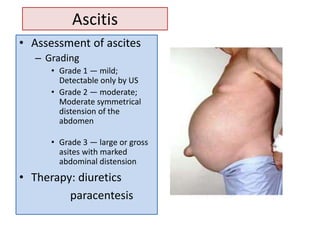
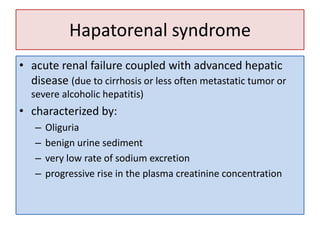
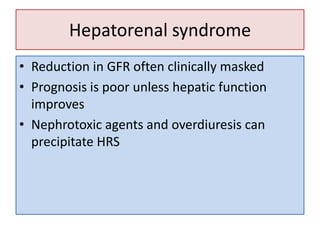
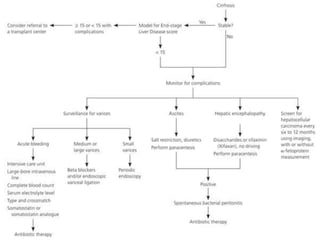
Cirrhosis is a consequence of chronic liver disease characterized by diffuse scarring and regeneration of the liver. It results from many causes including alcohol, viral hepatitis, and genetic conditions. As the liver architecture is disrupted, liver function declines and complications develop. Investigation of cirrhosis involves blood tests to assess liver function and damage, imaging to evaluate the liver structure, and potentially biopsy to determine the specific cause. Common complications arise from portal hypertension and include variceal bleeding, ascites, and hepatic encephalopathy. Cirrhosis can ultimately lead to liver failure and death without treatment or transplantation.