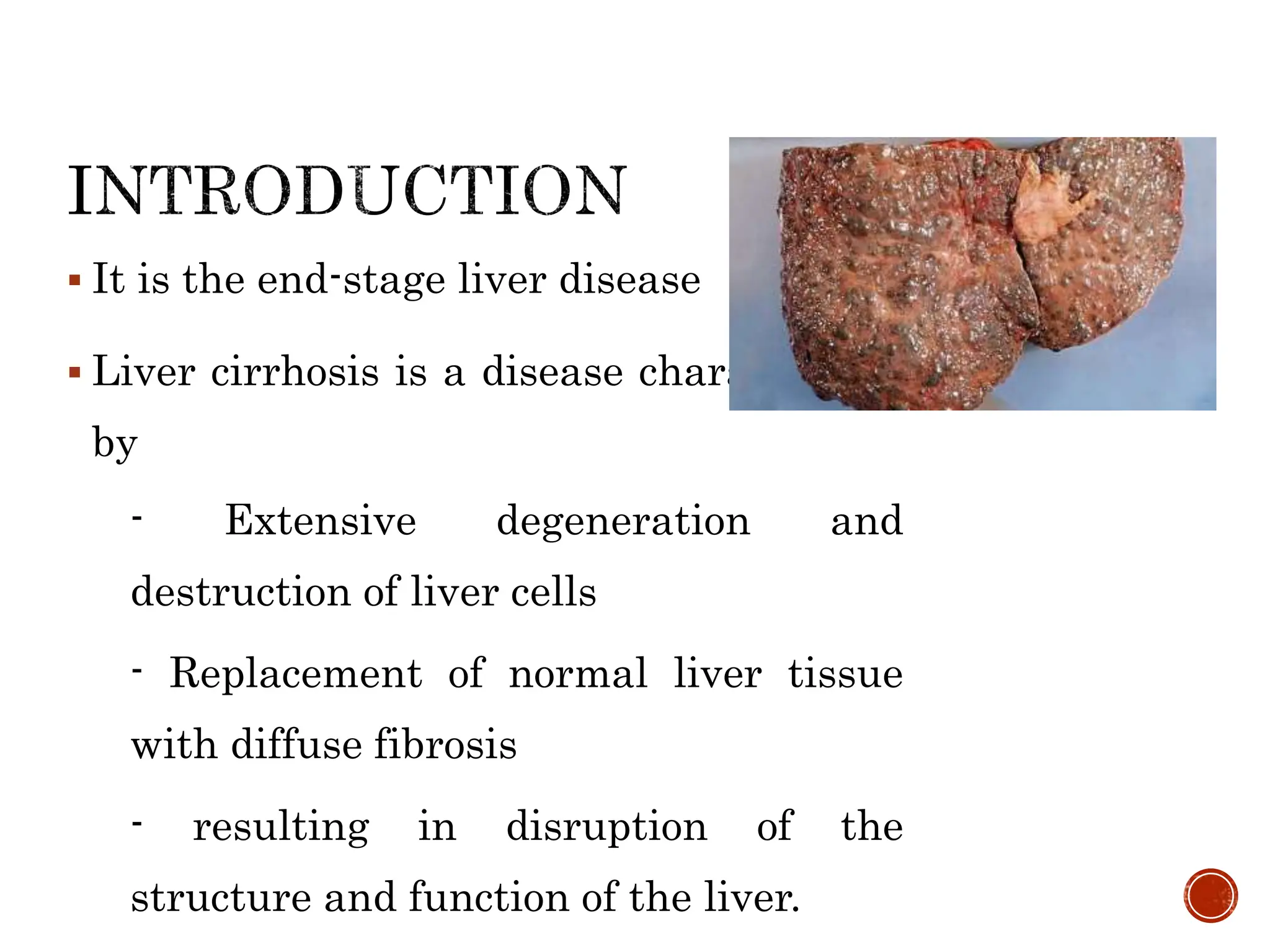
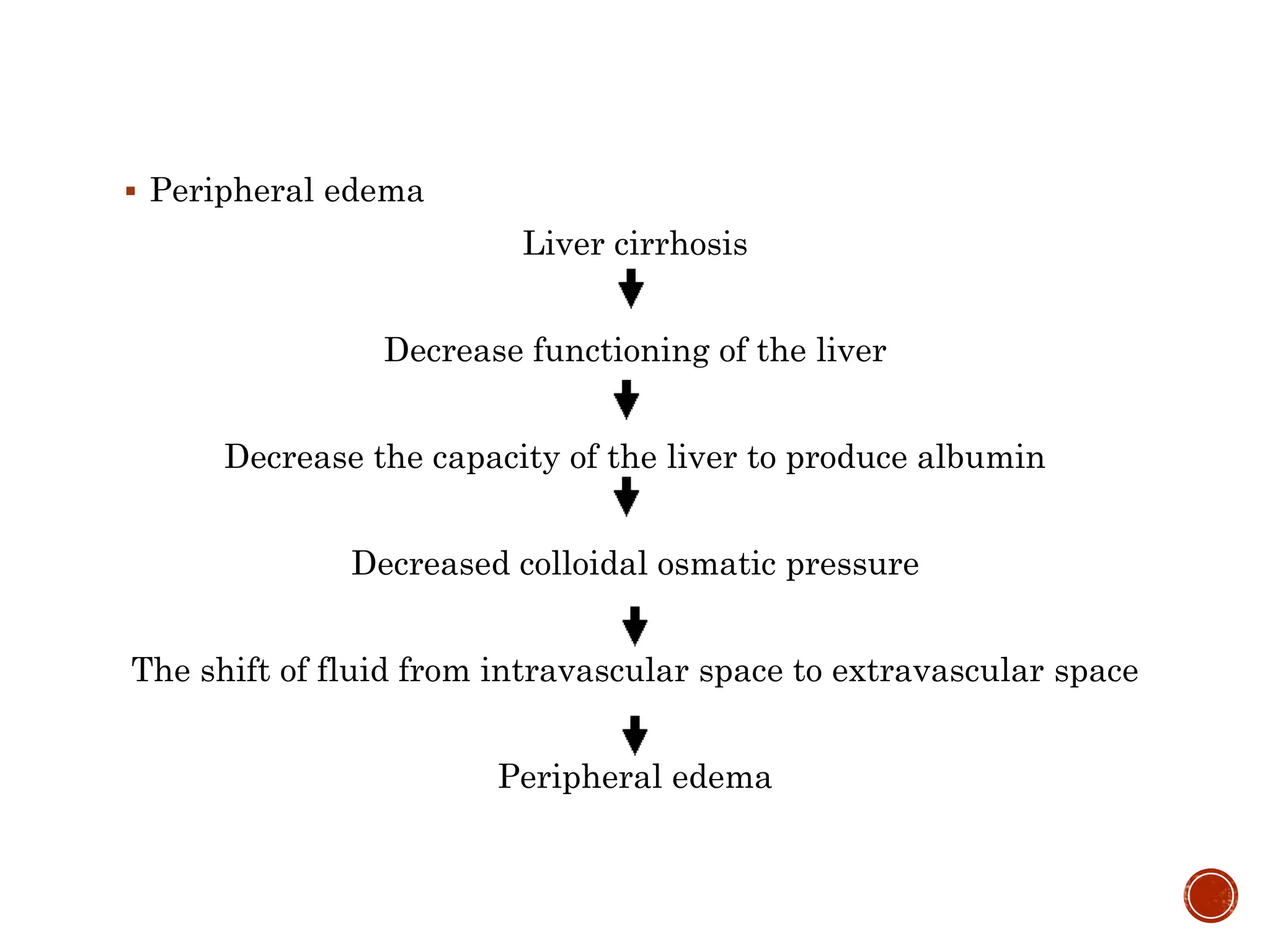
The document outlines a seminar on medical surgical nursing focused on liver cirrhosis, including its etiology, pathophysiology, clinical manifestations, and management strategies. It emphasizes the nurse's role in caring for patients with liver cirrhosis and highlights the importance of understanding liver anatomy, physiology, and related complications. Additionally, it discusses emerging therapies, particularly the potential for endothelial cell infusion to treat liver damage.