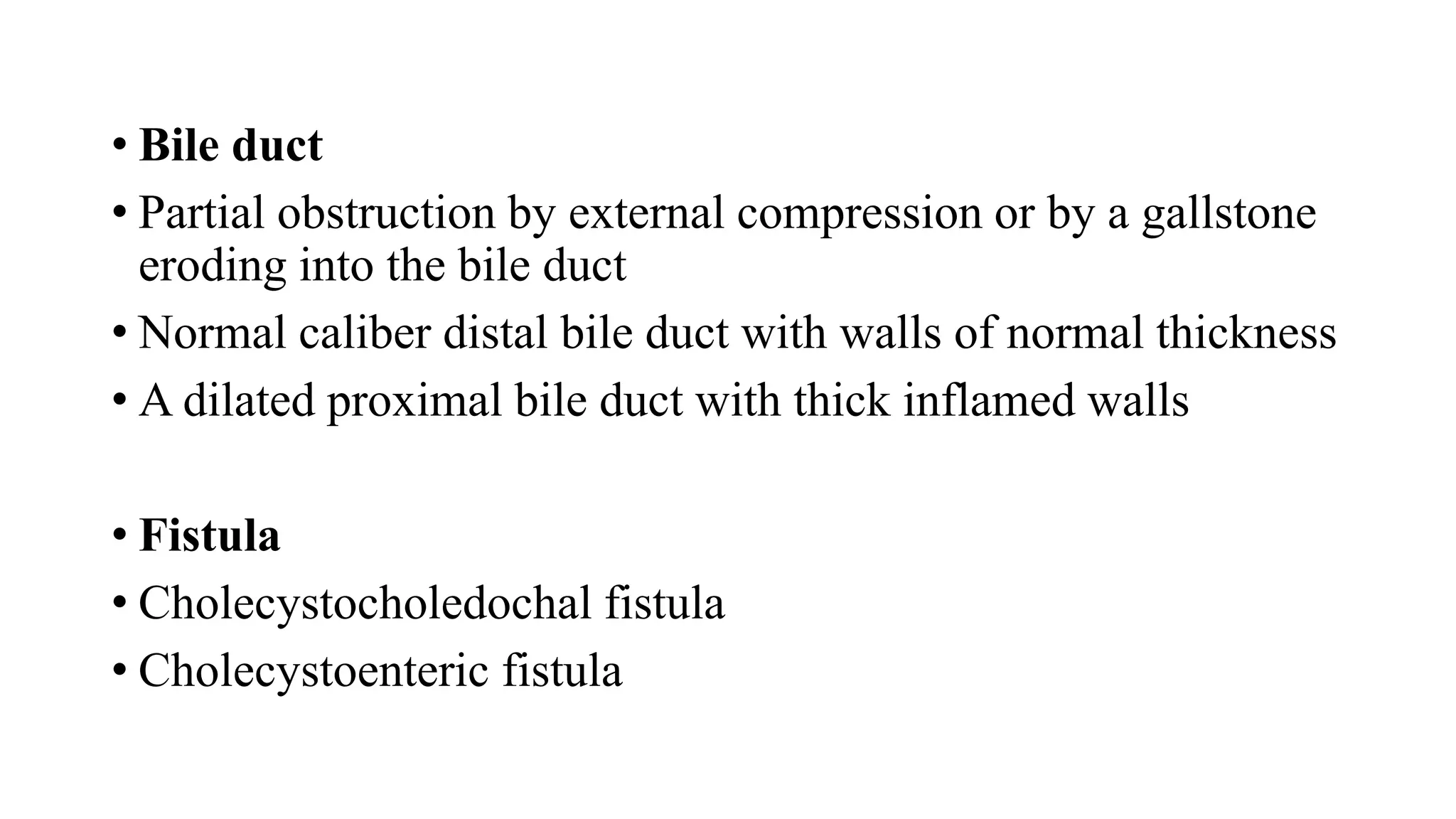
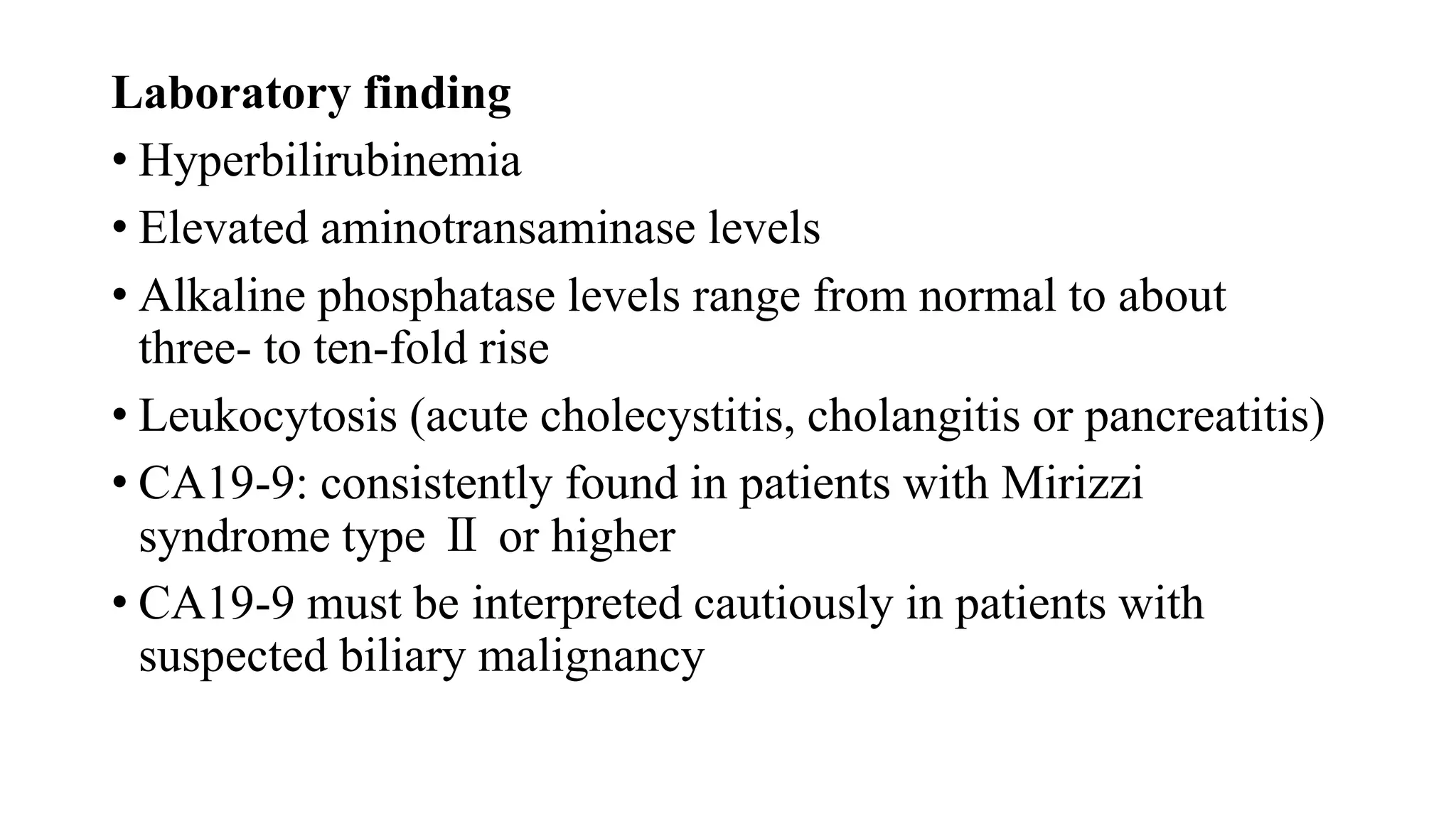
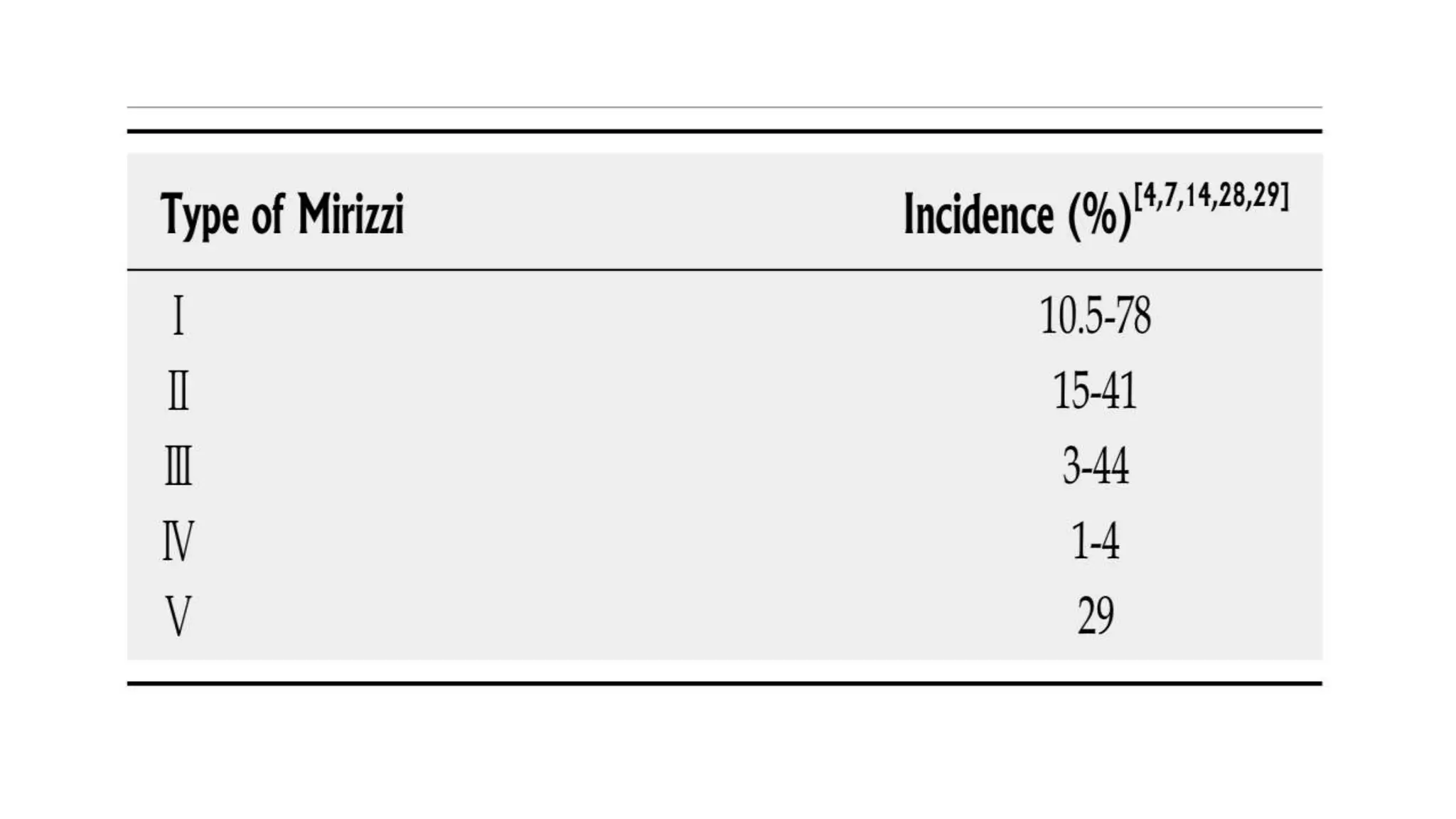
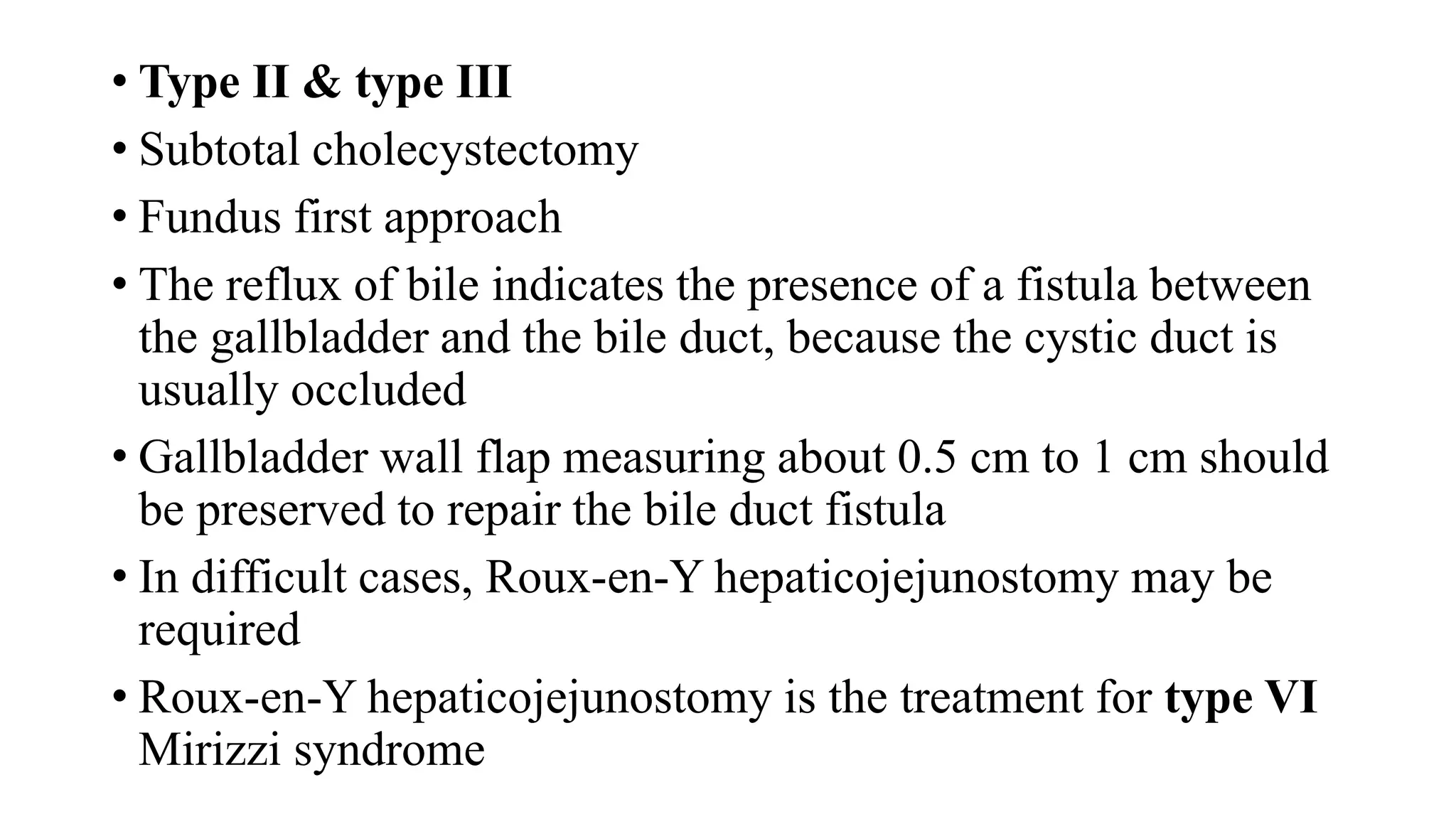
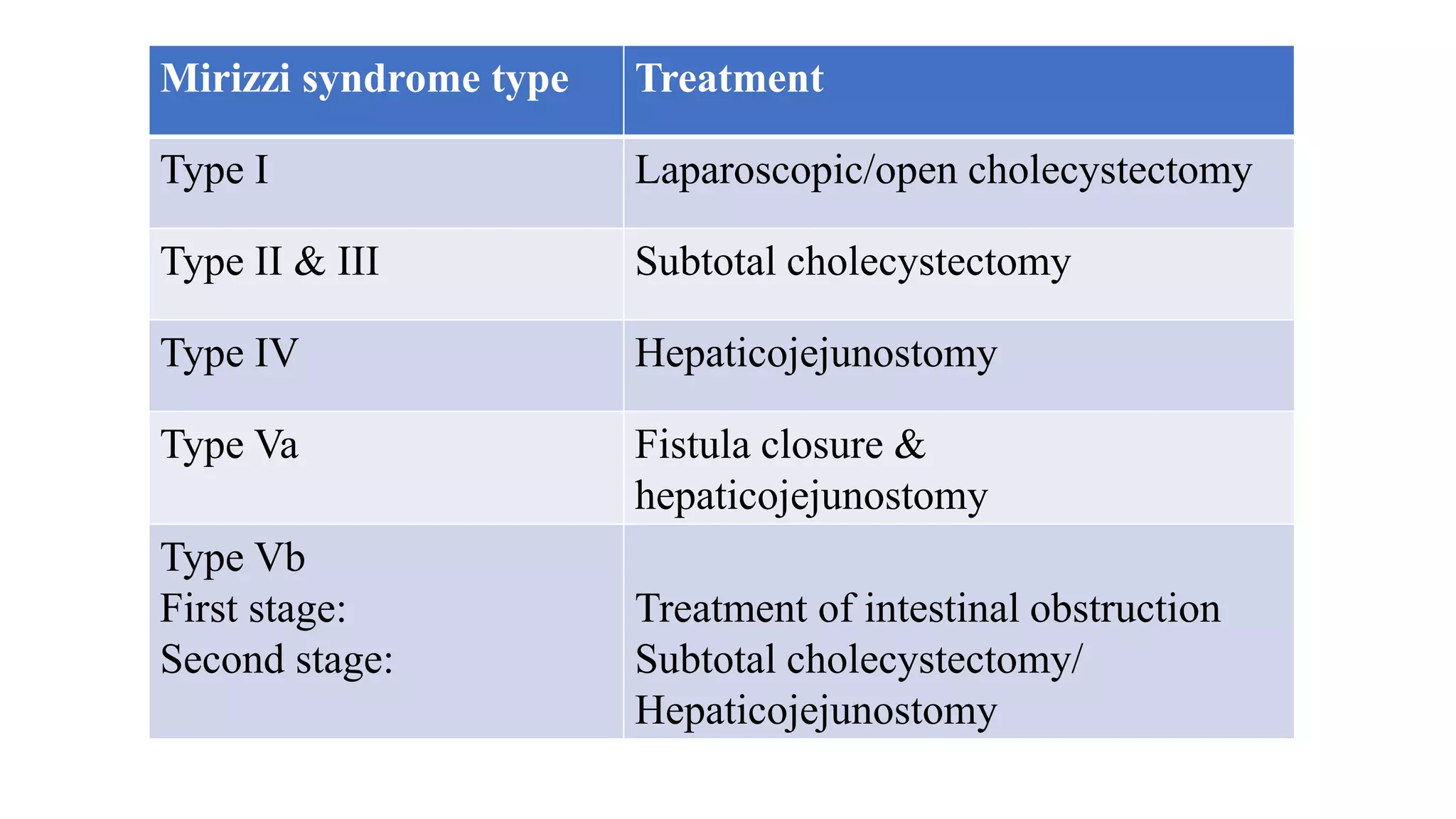
Mirizzi syndrome is a rare complication of long-standing gallstone disease that results in external compression or fistulization of the common hepatic duct by an impacted gallstone in the cystic duct or gallbladder. It occurs in 0.3-5.7% of cholecystectomy patients. Treatment depends on the classification type but may include subtotal cholecystectomy, fistula repair, or hepaticojejunostomy. Precise preoperative diagnosis is difficult but helps minimize complications like bile duct injuries during surgery for this condition with distorted anatomy.