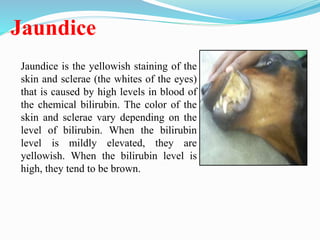
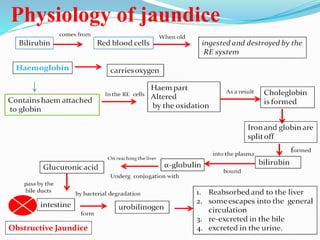
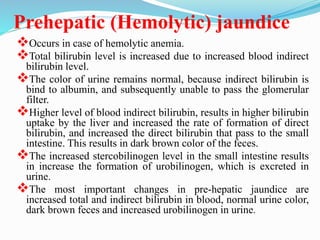
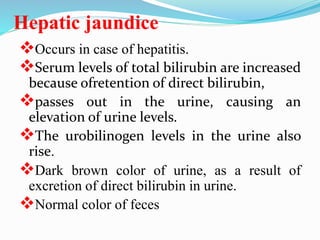
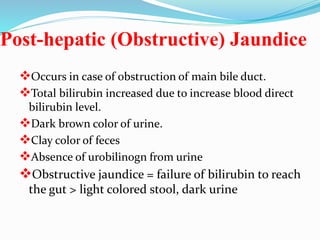
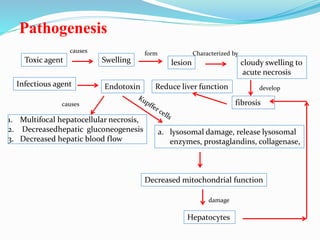
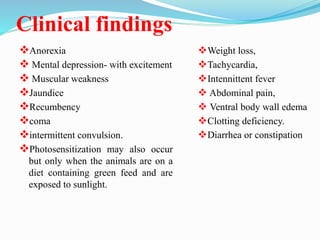
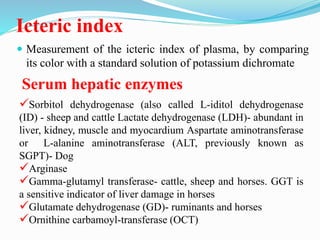
The document discusses hepatic (liver) functions and manifestations of liver disease. It covers topics such as jaundice, hepatic encephalopathy, and different types of jaundice (prehepatic, hepatic, post-hepatic). Liver diseases discussed include toxic hepatitis, infectious hepatitis, parasitic hepatitis, and nutritional hepatitis. Clinical signs, nervous system signs, and laboratory tests for assessing liver function and disease are also summarized.