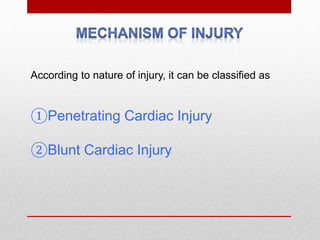
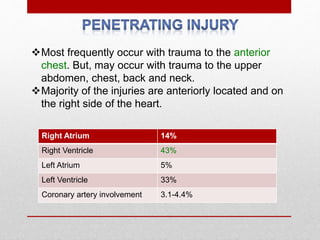
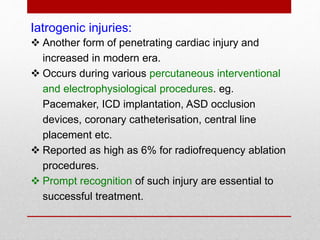
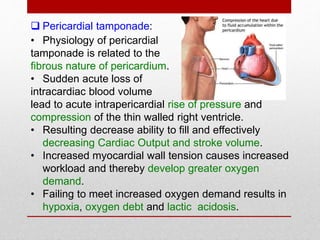
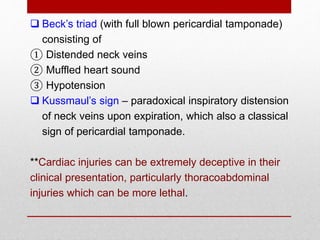
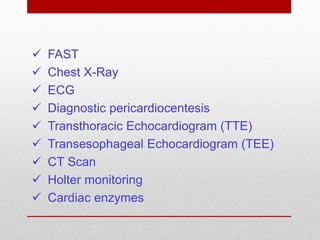
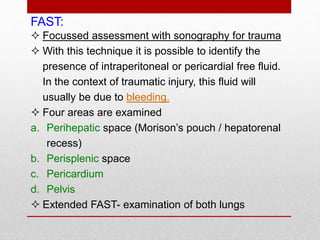
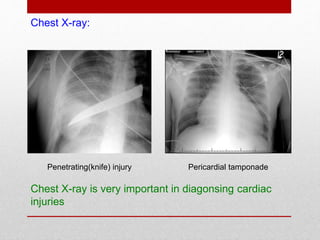
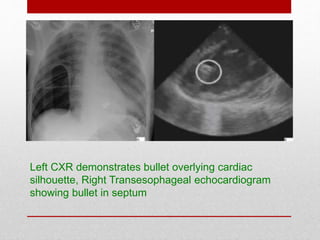
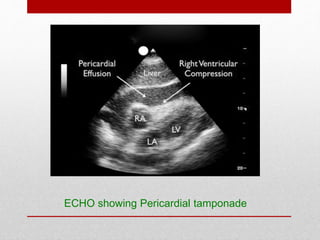
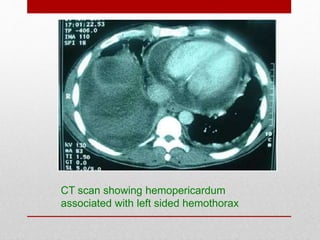
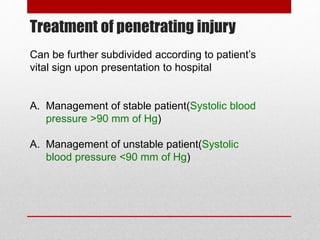
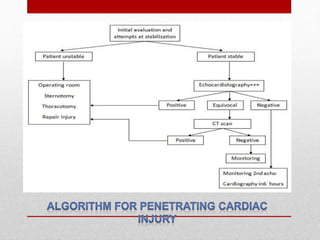
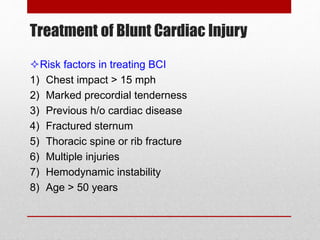
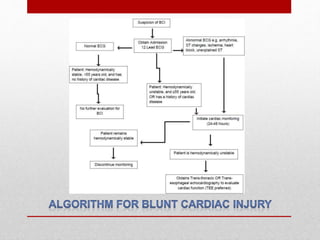
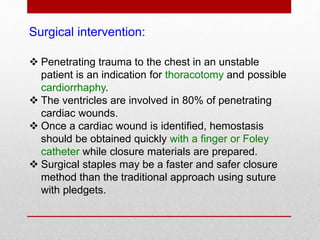
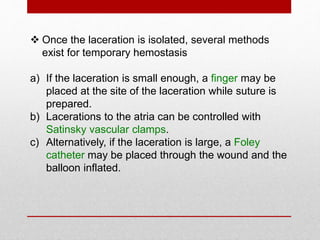
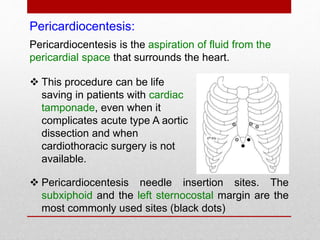
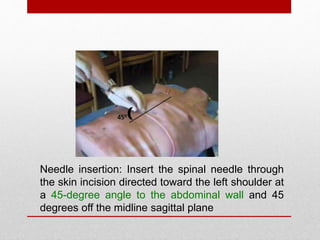
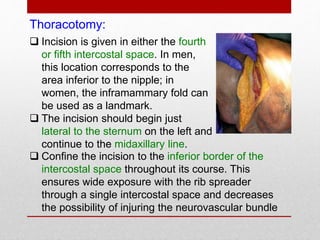
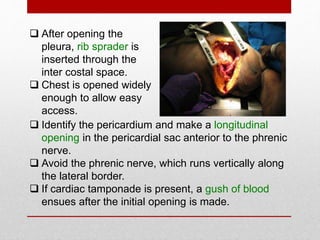
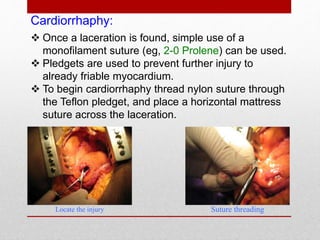
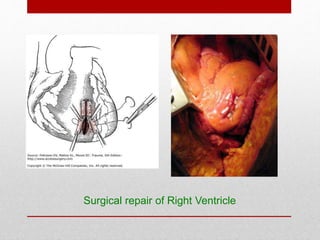
This document discusses recent advances in the management of cardiac trauma. It begins by noting that cardiac injuries continue to cause significant mortality despite improvements in trauma care. It then covers the classification, mechanisms, clinical presentation, diagnosis and treatment of both penetrating and blunt cardiac injuries. For diagnosis, it discusses tools like FAST exam, chest X-ray, echocardiogram and CT scan. For treatment, it outlines the management of stable versus unstable patients, describing surgical interventions like thoracotomy, cardiorrhaphy and pericardiocentesis.