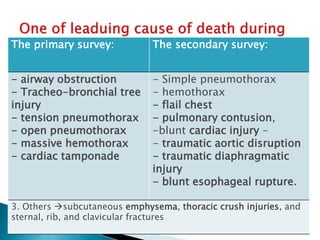
This document provides information on key topics in the management of chest trauma:
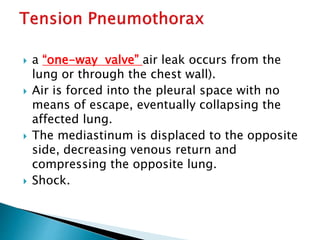
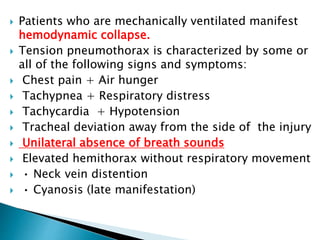
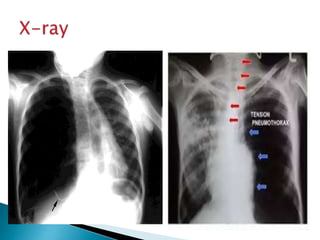
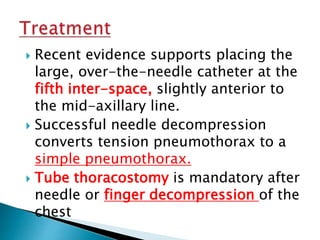
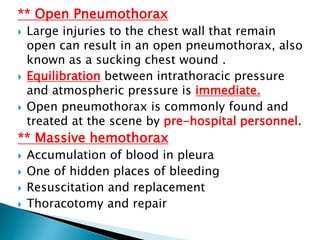
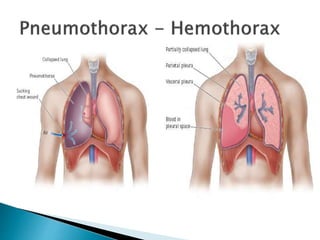
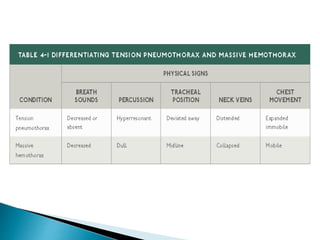
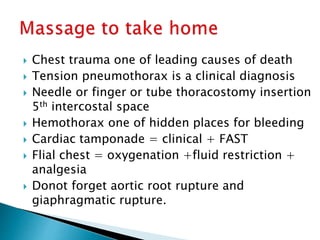
- Tension pneumothorax is a medical emergency diagnosed clinically and treated with needle or tube thoracostomy without delay.
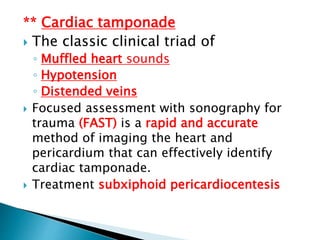
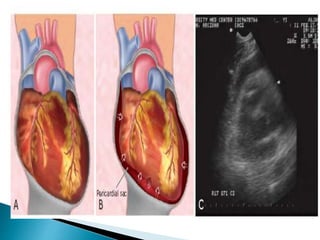
- Hemothorax over 1.5L or drainage over 200mL/hr requires tube thoracostomy or thoracotomy. Cardiac tamponade is diagnosed clinically and with ultrasound.
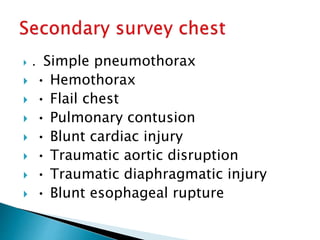
- Pulmonary contusions are managed with oxygenation, fluids restriction, and analgesia. Blunt cardiac injuries may cause hypotension or arrhythmias.


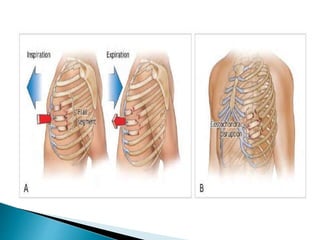
![ Abnormal respiratory motion and palpation of
crepitus from rib or cartilage fractures
Patients with significant hypoxia (i.e., PaO2 <
60 mm Hg [8.6 kPa] or SaO2 < 90%) on room
air may require intubation and ventilation
within the first hour after injury.
Associated medical conditions, such as chronic
requiring early intubation and mechanical
ventilation
Management
1. Ensuring adequate oxygenation
2. Fluids restriction
3. Providing analgesia to improve ventilation](https://image.slidesharecdn.com/chesttraumamibrahim-copy-190831105604/85/Chest-trauma-m-ibrahim-copy-21-320.jpg)
![1. Rhee PM, Acosta J, Bridgeman A, et al. Survival after emergency
department thoracotomy: review of published data from the
past 25 years. J Am Coll Surg 2000;190(3):288–298.
2. Stafford RE, Linn J, Washington L. Incidence and management
of occult hemothoraces. Am J Surg 2006;192(6):722–726.
3. Karmy-Jones R, Jurkovich GJ, Nathens AB, et al. Timing of
urgent thoracotomy for hemorrhage after trauma: a
multicenter study. Archives of Surgery 2001;136(5):513–518.
4. Simon B, Cushman J, Barraco R, et al. Pain management in
blunt thoracic trauma: an EAST Practice Management
Guidelines Workgroup. J Trauma 2005;59:1256–1267.
5. Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and
supine anteroposterior chest radiographs for the identification
of pneumothorax after blunt trauma. [Review] [24 refs] Acad
Emerg Med 2010;17(1):11–17.
6. Inaba K, Lustenberger T, Recinos G, et al. Does size matter? A
prospective analysis of 28-32 versus 36-40 French chest tube
size in trauma. J Trauma 2012;72(2):422–427.](https://image.slidesharecdn.com/chesttraumamibrahim-copy-190831105604/85/Chest-trauma-m-ibrahim-copy-27-320.jpg)