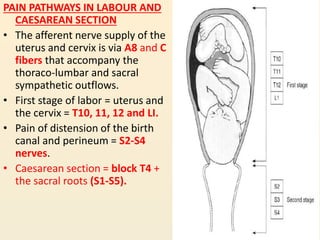
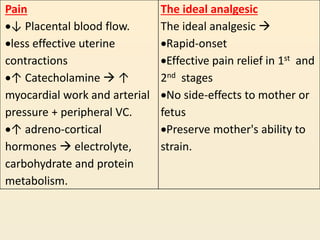
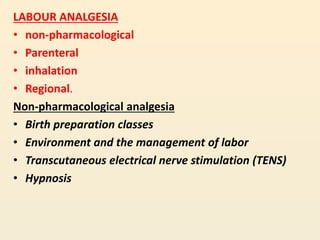
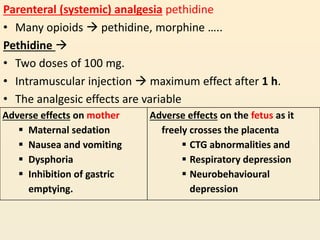
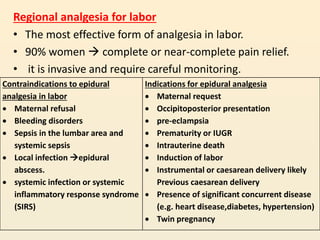
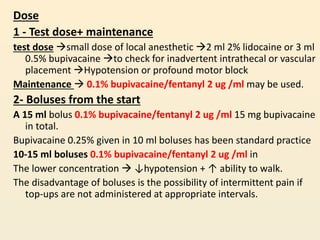
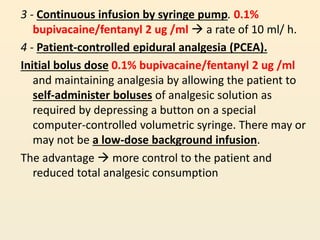
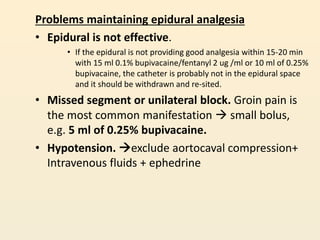
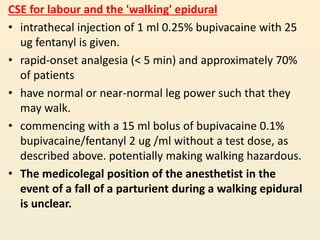
This document discusses pain pathways and methods of pain management during labor and caesarean section. It describes how the uterus and cervix receive nerve supply during different stages of labor. The ideal analgesic for labor should provide rapid and effective pain relief with no side effects to the mother or fetus. Methods of labor analgesia discussed include non-pharmacological techniques, parenteral drugs like pethidine, inhalation of nitrous oxide, and regional techniques like epidural analgesia. Epidural analgesia is described as the most effective form of pain relief but it requires careful administration and monitoring to avoid problems.