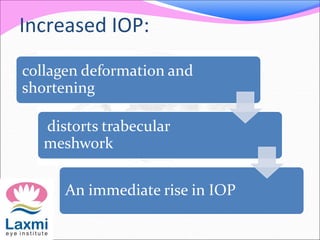
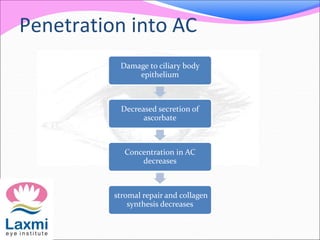
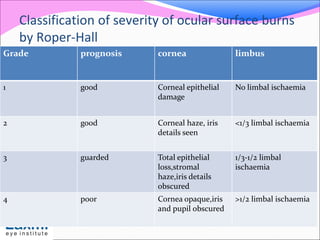
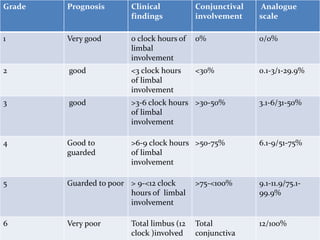
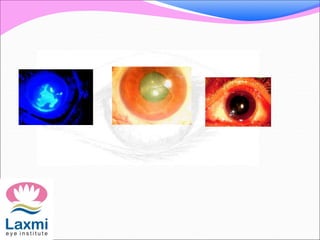
This document discusses chemical burns to the eye. It notes that both thermal and chemical burns can cause blindness. Common causes of chemical burns are cleaning products, fertilizers, cement, fireworks, battery acid, and bleach. Alkaline agents like these cause more damage than acids as they penetrate cell membranes and disrupt collagen. A classification system grades injuries based on extent of limbal ischemia and corneal haze. Treatment involves immediate and copious irrigation, controlling inflammation with steroids, promoting healing with artificial tears and ascorbate, and managing intraocular pressure. The goal is to remove the chemical, promote healing, prevent infection, and control inflammation.