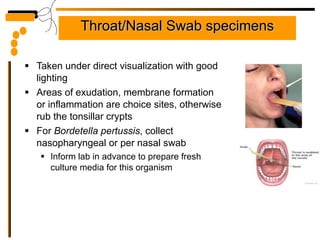
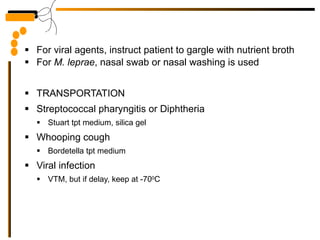
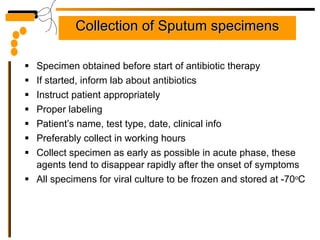
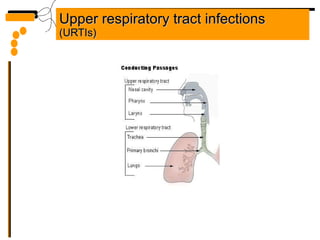
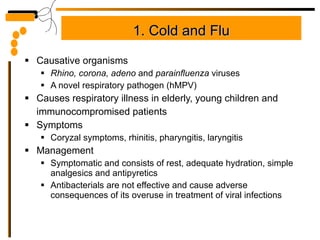
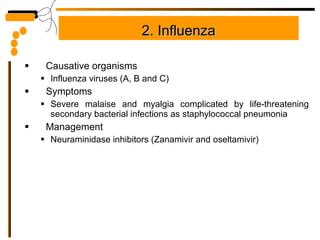
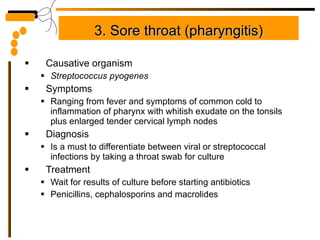
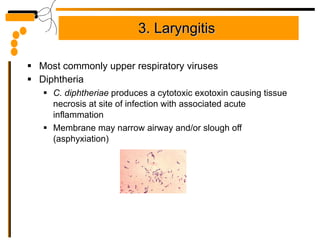
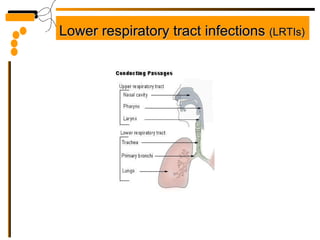
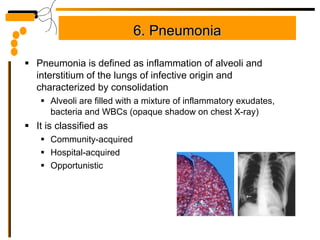
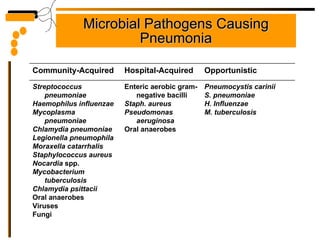
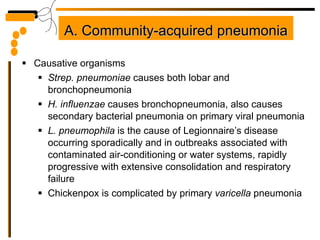
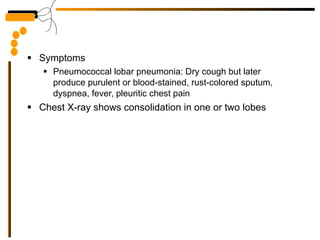
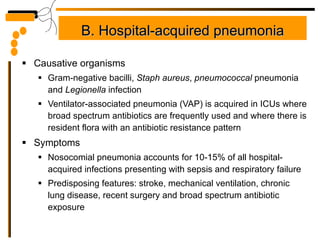
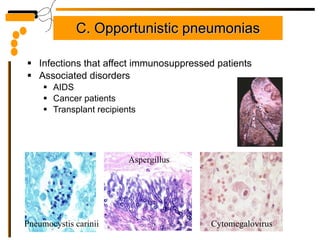
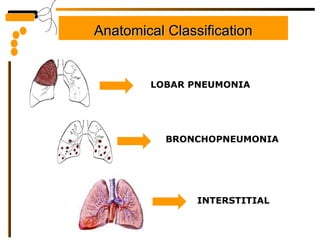
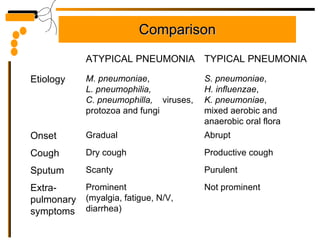
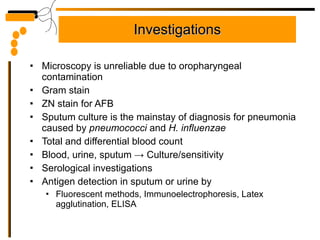
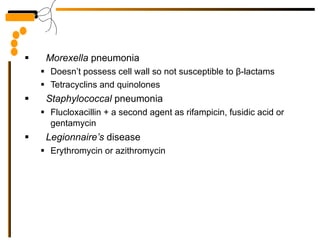
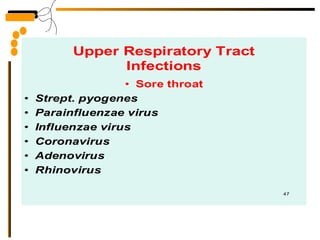
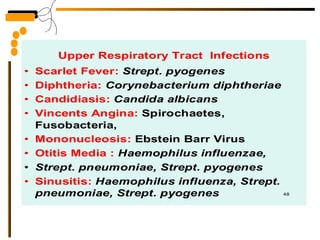
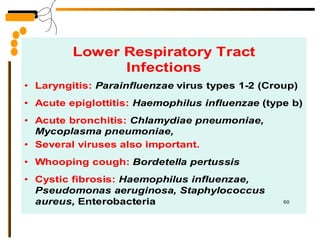
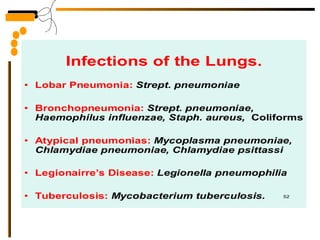
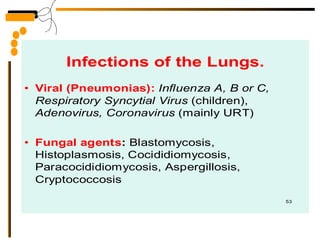
The document provides guidelines for collecting and transporting respiratory tract specimen for various infections, including proper labeling and storage. It describes common respiratory tract infections like pneumonia, their causes, symptoms, and treatment options. Pneumonia is classified as lobar, bronchopneumonia, or interstitial based on anatomical location and involvement; and as typical, atypical, community-acquired, or hospital-acquired based on etiology.