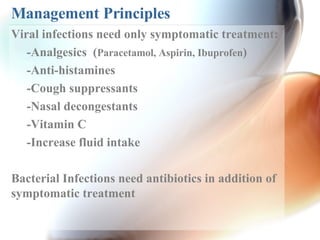
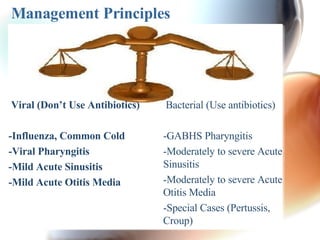
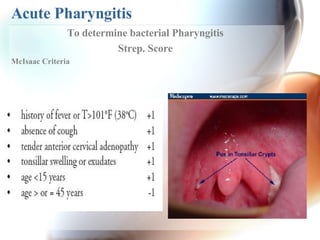
This document summarizes upper respiratory tract infections (URTIs) such as the common cold, acute sinusitis, acute otitis media, pharyngitis, and croup. It discusses the typical viral and bacterial causes, symptoms, management principles, and antibiotic treatment guidelines for each condition based on severity and risk of complication. For most viral URTIs, antibiotics are not recommended as they only provide symptomatic relief and promote antibiotic resistance. Bacterial infections like streptococcal pharyngitis may require antibiotics to prevent rheumatic fever or suppurative complications. Differentiating between viral and bacterial causes can be challenging, and tests like rapid strep tests or cultures may be needed before antibiotic prescription.