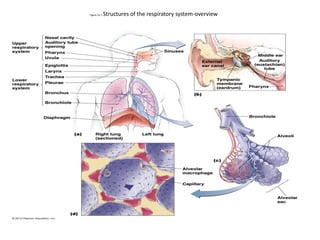
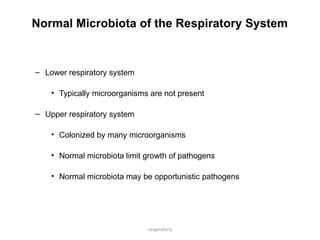
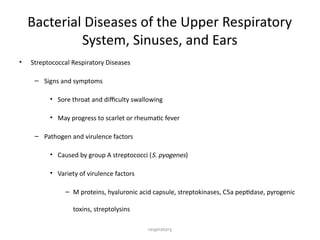
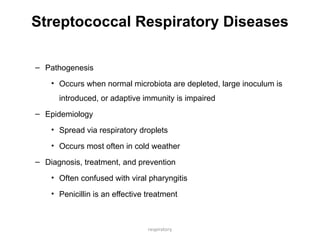
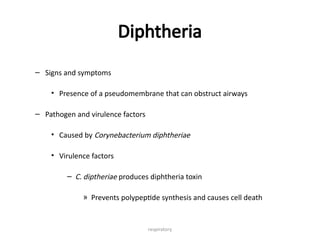
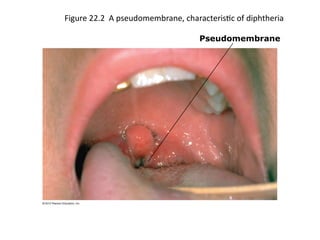
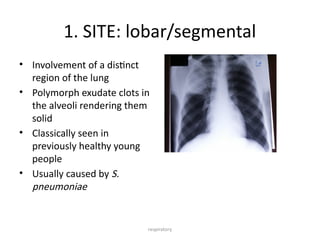
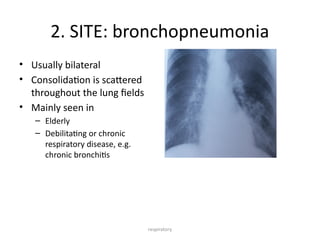
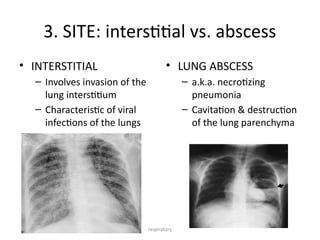
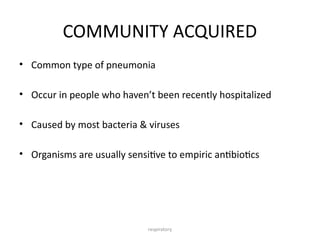
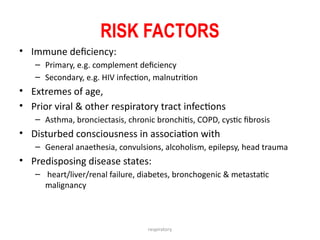
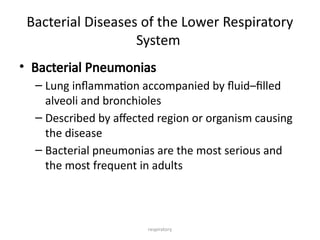
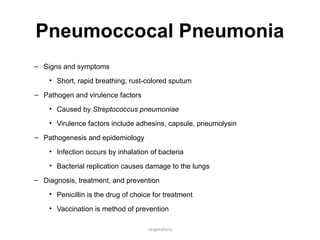
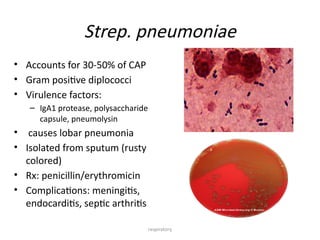
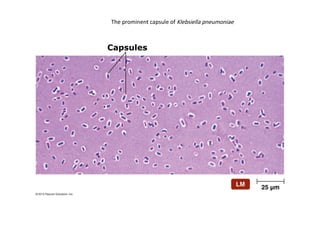
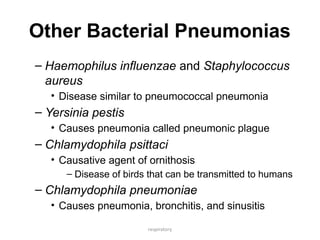
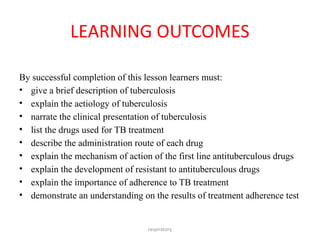
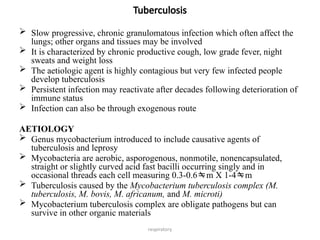
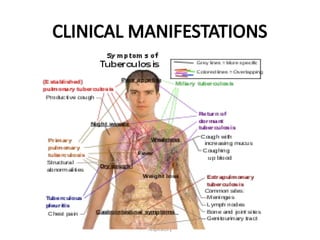
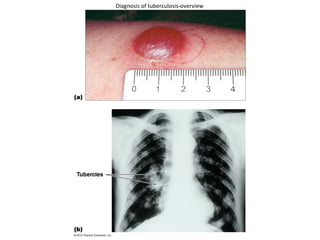
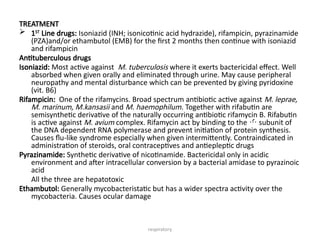
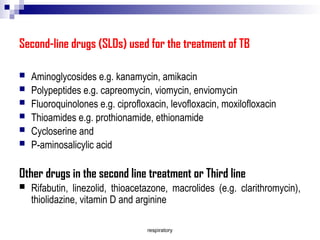
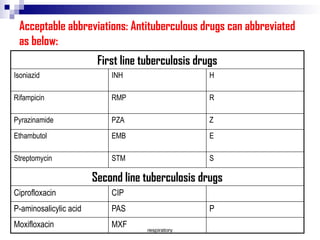
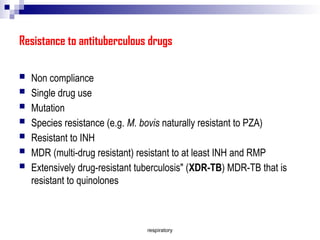
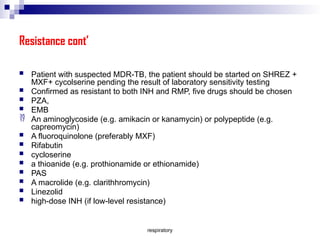
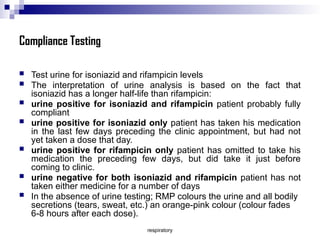
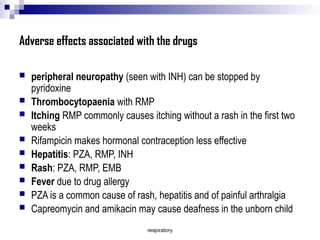
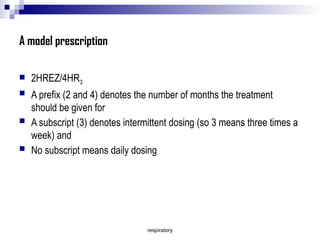
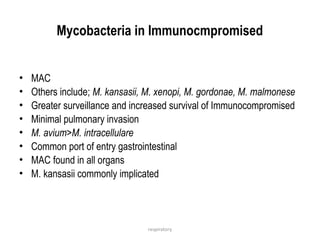
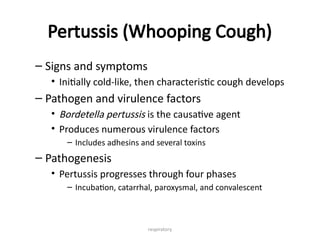
The document discusses diseases of the respiratory system, focusing on microbial infections caused by various pathogens, including streptococci, diphtheria, and tuberculosis. It elaborates on the anatomy, microbiota, pathogenesis, symptoms, treatment, and prevention of these conditions including pneumonia classifications and resistance to tuberculosis drugs. The content also highlights the importance of compliance in treatment and the potential adverse effects associated with antituberculous medications.