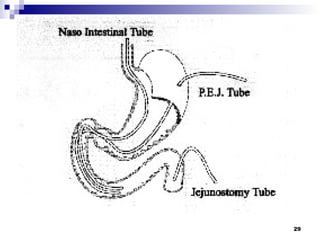
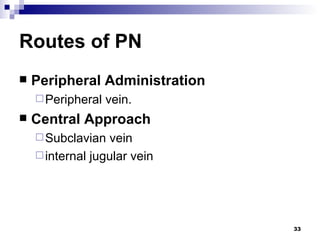
This document discusses surgical nutritional support, including the history and importance of artificial nutrition, metabolic adaptations in catabolic states, nutritional assessment, and approaches to enteral and parenteral nutrition. It covers indications for nutritional support, routes of administration, considerations for formulas including calorie-nitrogen ratios, and potential complications of enteral and parenteral nutrition administration. Metabolism in stress and starvation states and the regulation of protein synthesis and degradation are also summarized.











![General Indications for Nutrition Support and Choice of Route of Administration The pre-morbid state (healthy or otherwise) Poor nutritional status (the current oral intake meets <50% of total energy needs) Significant weight loss (initial body weight less than the usual body weight by ≥10%, or a decrease in inpatient weight by >10% of the admission weight) The duration of starvation (>7 days' inanition) An anticipated duration of artificial nutrition (particularly for total parenteral nutrition [TPN]) of more than 7 days The degree of the anticipated insult, surgical or otherwise A serum albumin value less than 3.0 g/100 mL measured in the absence of an inflammatory state](https://image.slidesharecdn.com/surg-nutritional-supp-1231172773837431-2/85/Surg-Nutritional-Supp-12-320.jpg)






![Harris-Benedict equation BEE = 66.5 + (13.7 X weight [kg]) + (5.0 X height [cm]) - (6.8 X age [yr] [male]) BEE = 655.1 + (9.56 X weight [kg]) + (1.85 X height [cm]) - (4.68 X age [yr] [female]) (BEE = basal energy expenditure)](https://image.slidesharecdn.com/surg-nutritional-supp-1231172773837431-2/85/Surg-Nutritional-Supp-19-320.jpg)