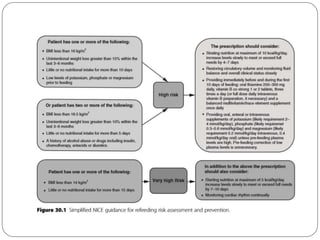
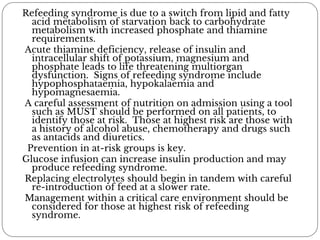
A woman with a history of anorexia nervosa and a BMI of 12 kg/m2 was admitted for investigation of weight loss. She deteriorated after initiation of enteral feeding and dextrose infusion, presenting with respiratory failure, hypotension, arrhythmia, and metabolic abnormalities. Given her history of malnutrition and rapid change in nutritional status with feeding, she had likely developed refeeding syndrome, a condition caused by shifts in electrolytes and metabolism during the reintroduction of nutrition to a malnourished patient. Proper identification of high-risk patients and gradual, monitored refeeding is key to preventing refeeding syndrome.
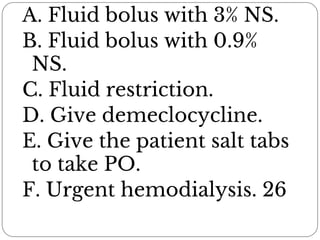
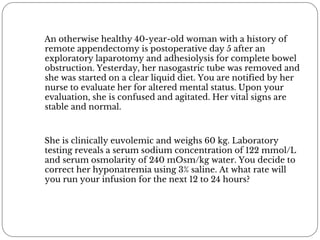
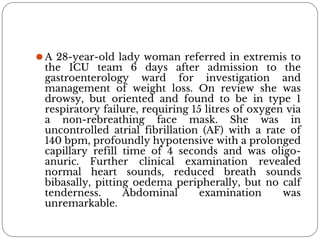
![3% Saline= 513 mmol/L of sodium Patient's
serum sodium= 122 mmol/L TBW=30
Change in serum [Na] = (513 - 122)/(30 + 1) =
12.7 mmol
A safe target for correction of serum
sodium is 10 mmol in 24 hours. For this
patient, a correction of 10 mmol would take
790 mL ( 10/12.7 =. 79). To infuse 790 mL
over 24 hours would take a rate of 33 mL/h](https://image.slidesharecdn.com/fluidincriticallyill-191115081218/85/Fluid-Therapy-in-critically-ill-6-320.jpg)